Busier surgeons have better outcomes, the future of handshakes, artificial Intelligence and health care costs, and annual COVID-19 vaccinations.
January 27, 2022:
Happy Friday!
Today, I’ll discuss a new study that makes it clear that orthopedic surgeons who do more procedures have better outcomes and lower costs, review whether handshakes are a “good idea,” and discuss the impact of Artificial Intelligence (AI) on medical costs. I’ll also review last night’s FDA recommendation on annual COVID-19 vaccinations.
1. Orthopedic surgeons who perform more total joint replacements have better outcomes and lower costs.
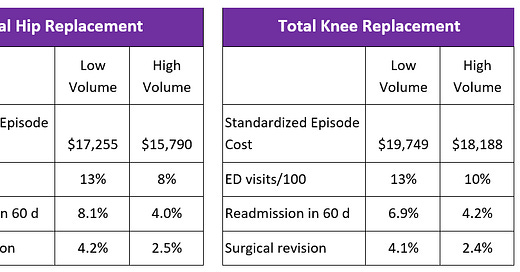
Researchers at Clarify Health, a software and analytic company, reported last week that their review of claims data shows that orthopedic surgeons who performed more than 100 hip or knee replacements on those insured by commercial payers from 2017 to 2020 had dramatically better outcomes and lower costs in 2021 than low-volume orthopedic surgeons, who performed fewer than 10 procedures. The sample was over 66,000 hip replacements and 110,000 knee replacements, about 1 in 7 procedures performed in the US. The majority of hip and knee replacements are done on those over age 65 and are covered by Medicare, and these were not included in this study. The researchers standardized costs and controlled for other medical conditions.
Source: Clarify Health January, 2022 LINK
Implications for employers:
- Members gain the most value from having major orthopedic procedures performed by surgeons who perform many similar procedures.
- This shows the value of Centers of Excellence (COE), although some surgeons within a COE might themselves be low-volume surgeons.
- Employers should promote transparency initiatives to inform patients about surgical volume when they are deciding which surgeon to consult.
2. Should we shake on it?
Image generated by Dall-e of OpenAI www.openai.com
At the beginning of the pandemic, one epidemiologist told the New York Times, “Real epidemiologists don’t shake hands.” In March, 2020, we didn’t know much about how COVID-19 was transmitted between people, and we thought avoiding handshakes could protect us from COVID-19 based on real-world experience with influenza, RSV, and other respiratory diseases.
Researchers have since found that hands (and doorknobs and railings) are not frequently responsible for spreading COVID-19. The coronavirus can be cultured from hands (or surfaces), but is rarely the cause of COVID-19 spread. The coronavirus is largely spread through the air, so wearing a mask provides more protection than avoiding a handshake.
So - should we shake hands?
Handshakes are an important salutation. They help create social and business bonds, and they help us restore a sense of normalcy in a world that sometimes seems disordered and threatening. So, I’m back to shaking hands with mutual consent. I recognize that a handshake can easily spread influenza, RSV, and norovirus -so I won’t be offended if some people don’t want to take the risk of shaking my hand. Elbow and fist bumps can help confirm important relationships, too.
As we return to handshakes, we can make handshakes safer by washing hands well. We can cough or sneeze into our elbows (and not our palms!), and we can stay out of public places when we are sick.
My Apple Watch telling me I should wash my hands longer.
Implications for employers:
- Make hand sanitizer widely available, especially during gatherings where handshaking is more common.
Source: Panch, et al PLOS Digital Health May, 2022 LINK
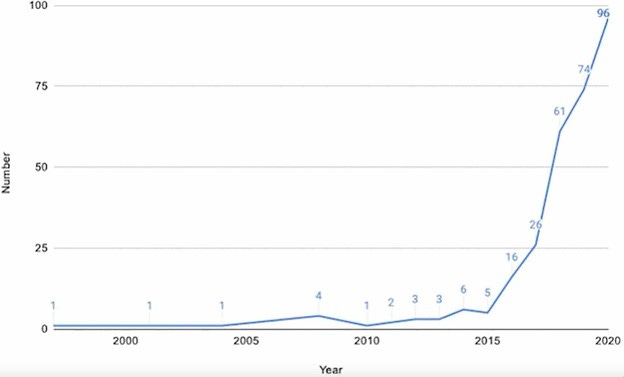
3. Will Artificial Intelligence (AI) solve our health care cost crisis?
A preeminent economist and three consultants published a report this week suggesting that use of artificial intelligence could decrease medical costs by 5-10%, using technology already available and fully implementable in the next 5 years. The authors state that these savings would be about 40% from administrative savings (9-19% of administrative costs) and 60% from reducing medical costs (4-8% of medical costs). For instance, using machine learning and natural language processing could allow effective risk prediction from narrative in electronic medical records, allowing us to focus our attention on patients where we can make the most difference. Hospitals could improve efficiency in scheduling and in supply chain management. Health plans could automate their member services and prior authorizations, while hospitals could automate some customer service functions.
The authors are clear that they have not included the initial capital cost of incorporating AI in medical and administrative processes in medical care. Indeed, the adoption of AI could increase total health care costs over the coming years. AI systems are trained on real world data, which incorporates substantial structural racism. So we will need to guard against inadvertently increasing existing disparities.
Finally, I’m worried that some of these administrative savings will be lost as we initiate an ever-escalating AI battle. For instance, insurers can use AI to automate prior authorization - but what if providers implement AI, too? Will “battling bots” actually lower health care costs? One study published this month shows that the “hassle factor” of prior authorization lowers medical costs, so automating prior authorization could paradoxically raise costs! Further, the promise that IBM Watson would revolutionize oncology care proved premature, and providers are likely to move slowly and require substantial validation before implementing AI and machine learning in clinical practice. On the other hand, here’s an example of using Chatbots to increase pediatric touchpoints and increase childhood vaccination in a poor neighborhood in Chicago.
I suspect that we will see substantial incorporation of AI and machine learning that will decrease waste in health care, but adoption will be slower than the authors project, and in many instances, the savings will be realized by providers or health insurance plans, and not by employers which sponsor health insurance plans.
Implications for employers:
- We should continue to pursue many approaches to controlling health care costs.
- Hopefully, AI will help - but let’s not count on this technologic revolution lowering health care costs.
I’m giving AI the last word here. I asked the AI bot CHAT GPT3 to predict whether AI would lower health care costs. This Chatbot was trained on the internet as of late 2021, so the current article was not part of the training database.
Generated by CHAT GPT3 on January 23, 2023 available at www.chat.openai.com
4. FDA recommends each COVID-19 vaccine have a single formulation
A Food and Drug Administration advisory committee met yesterday to evaluate how to move forward with COVID-19 vaccinations. The question before the FDA was whether vaccine manufacturers should “harmonize” primary vaccinations and boosters. The committee voted unanimously in favor of each vaccine having a single formulation, which would likely be an annual shot for most, and could be more frequent for the elderly, young children, and those at highest risk. The new harmonized shot would likely be bivalent, although the actual composition and timing for shots would be determined this spring.
Current vaccination recommendations are too complex. For instance, children under five need a primary series of three Pfizer or two Moderna shots, which are not interchangeable. There is still no booster at all available for those who had a primary Novavax series. A simpler set of rules will help make vaccination manageable and may increase shots in arms.
Many questions remain about the future approach to COVID-19 vaccination. Uptake of the bivalent booster remains low (about 16% of those eligible.) Many scientists remained concerned that we don’t yet know if there will be a “season” for COVID-19, and therefore cannot tell the optimal timing for future vaccinations. Lastly, while current vaccines are effective, their protection does not last 12 months. This means that an annual vaccine may not come out when it is most needed.
Many experts advocate putting more resources into vaccines that provide long-term immunity. A vaccine against the coronavirus’ nucleotide protein, which mutates less than the spike protein, or a nasal vaccine, which could decrease transmission by preventing infections through upper respiratory immunity, could be more effective than the current vaccines.
Implications for employers:
- A simpler set of rules could help increase vaccination rates and support employers’ campaigns to encourage their workforce to be immunized. COVID-19 vaccines will become the financial responsibility of employer-sponsored health plans in the near future, and their cost will increase dramatically.
· Employer-sponsored plans that are compliant with the Affordable Care Act will cover vaccinations recommended by the CDC’s Advisory Committee on Immunization Practices (ACIP) will be covered with no cost sharing.
Sources for this section: Food and Drug Administration, StatNews, New York Times, Wall Street Journal, Katelyn Jetelina
Have a great weekend!
Jeff




Totally agree with the research on surgeons. I think Leapfrog had stats about the correlation of complication rates and number of procedures in a hospital. So makes total sense about surgeons too. I would suggest a well oiled and highly functional surgical team include the rehab team contributes to the success rates as well (spoken from someone who has recently received a new hip). And welcome back to the handshaker club. We missed you!!!