New cases of cardiovascular disease (CVS) in those under 40 by smoking status
Source: Franklin, et al Epic Research Network, April 30 2024 LINK
Heart disease decreased dramatically between 1980 and 2010. When I was in training, I frequently treated men in their 40s and 50s, almost always smokers, with life-altering or life-ending heart attacks. Heart disease rates declined as fewer smoked and better blood pressure and cholesterol medicines became available. Cardiologists also were able to treat symptomatic people with angioplasty, so rates of invasive coronary artery bypass surgeries went down.
However, there are two recent studies with unsettling news.
The Epic Research Network reviewed its extensive electronic medical record warehouse from 2010-2023, and found that the rate of cardiovascular disease among those under 40 doubled (from 9.4/1,000 to 22/1,000). Rates tripled for smokers under 40 (10.2/1,000 to 30.2/1,000). Among nonsmokers, rates of cardiovascular diagnoses increased even among those who were not overweight or obese. Researchers had access to over 25 million patient records for this analysis.
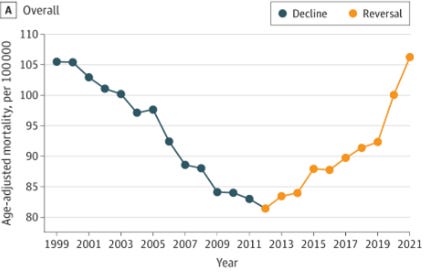
JAMA Cardiology reported that from 1999-2012, age-adjusted deaths from heart failure declined. Rates started to rise that year and deaths increased further during the COVID-19 pandemic. The death rate from heart failure is now higher than it was in 1999. These researchers used death certificate data, which is not as reliable as medical records, but this finding is especially worrisome. Rates of death from heart failure almost tripled in those under age 45 (1.2 to 3.2/100,000) and increased by 50% for those ages 45-65 (33/100,000 to 48/100,000).
Death Rate from Congestive Heart Failure, 1999-2021
Source: Sayed, JAMA Cardiology April 24, 2024 LINK
Implications for employers:
This data highlights the importance of supporting members to quit tobacco smoking; the rates of premature heart disease among smokers are high and rising more rapidly.
Improved blood pressure control can help prevent premature heart disease, and data from health plan reporting shows that the rate of effective control of blood pressure in those with known heart disease has not improved in the last two decades.
COVID-19 caused substantial vascular inflammation, but these trends were well established before the pandemic.
Employers may want to think about programs to address CVD risk factors as ways to mitigate this trend, particularly obesity and diabetes.
This is an example where increased population illness could be the cause of higher future medical costs.
Thanks for reading, and please subscribe and let others know about Employer Coverage!
Monday: GI side effects from GLP-1 anti-obesity drugs