Changes in Provider Billing, Anniversary of COVID-19 Emergency, Provider Directories, and Delaying Medical Care for Serious Conditions
March 17, 2023
Happy Friday,
Today, I’ll review some data on changing provider billing patterns, talk about what we’ve learned in the three years since the initial Pandemic Emergency was declared, present some worrisome data about insurer provider directories, and show some concerning information about Americans delaying medical care for serious conditions.
But first, a shameless plug. I had an opinion piece in StatNews yesterday, urging the White House to include economists and finance experts in the Cancer Moonshot to be sure that new approaches will be affordable. Read it here.
1. Providers are billing for higher levels of care, which worsens our unit cost problems
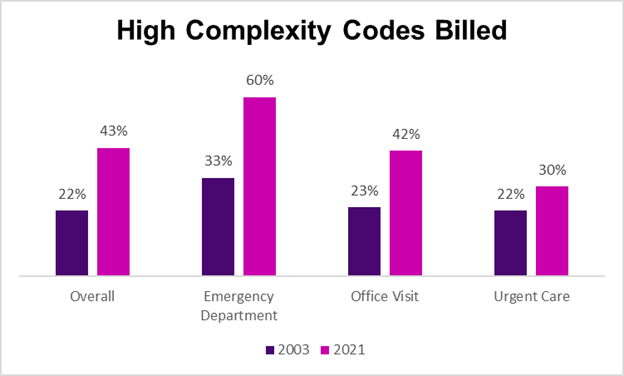
Researchers from Kaiser Family Foundation examined data from the Merative Marketscan database (previously called IBM Watson) and found that provider billing for cognitive services has shifted dramatically over the last 18 years. Providers have billed higher intensity codes for their services in emergency departments, office visits, and urgent care visits. This holds true even when looking at bills for specific conditions.
Source: KFF Peterson Health System Tracker February, 2023 LINK
The researchers note that this could mean that patients got substantially sicker, but this is unlikely. This increase is probably related to provider pressures to increase revenue and the ability to create documentation supporting higher level office visits using electronic medical records. Upcoding makes health care more expensive for employers, and often increases out-of-pocket costs due from members.
Implications for employers:
- The US health care system is more expensive than other developed countries largely because our costs per unit are dramatically higher. This apparent upcoding makes the situation worse.
- Employers should expect carriers to strictly police the most blatant examples of upcoding, and to effectively investigate when data analytics identifies providers who appear to be billing inaccurately.
- Some health plans have instituted automated “downcoding” programs, although these have commonly been challenged in court.
2. What we’ve learned from three years of the COVID-19 pandemic
It’s been three years since the COVID-19 Emergency declaration of March 13, 2020. We know much more than we knew back in Spring, 2020, and we are dramatically safer. A few thoughts on some pandemic lessons.
A) Science delivered.
We got effective vaccines under a year after the coronavirus was genetically sequenced, and a rapid-fire set of monoclonal antibodies and oral medications to treat COVID-19.
B) Science is not static.
We have learned that COVID-19 is transmitted in the air, so all our disinfection of mail and groceries was a waste. Public health officials discouraged masks early in 2020, but we later learned that they work well to protect individuals. We all need to be humble - facts we think we know today might turn out to be wrong tomorrow!
C) Public policy should not be static.
Vaccine mandates were a good idea when instituted in 2021, when they accelerated vaccine adoption. But vaccine mandates do little to prevent workplace transmission in 2023 and can be discontinued by most employers.
D) Work can change.
The pandemic brought us many changes in work that were likely overdue. We figured out how to make video conferencing work, and business prospered even with dramatically decreased business travel. Employees benefit from greater flexibility, and employers benefit from a much larger potential pool of talent.
E) Medical care can change, too
Providers pivoted to remote care, and mental health care access increased during the pandemic. Medical journals published research quickly and took down paywalls for pandemic-related articles. Hopefully, we’ll continue to gain value from these interventions even as the pandemic recedes.
F) Indoor air quality matters
Not only can better ventilation prevent COVID-19 transmission, but it can also protect against influenza and other viruses, and it can improve cognition and productivity
G) Government and the private sector can work together effectively
The pandemic required exceptional coordination between the government, which acquired COVID-19 vaccinations and drugs, and employers, which provide health insurance for 150 million Americans.
H) We should be prepared for future pandemics
Our changing climate allows increased spread of diseases once limited to tropical zones, and avian influenza continues to threaten to spill over into humans. Companies have reassessed their supply chains, and need to continue to be ready for future infectious disease challenges.
3. Provider directories remain inconsistent even after the No Surprises Act
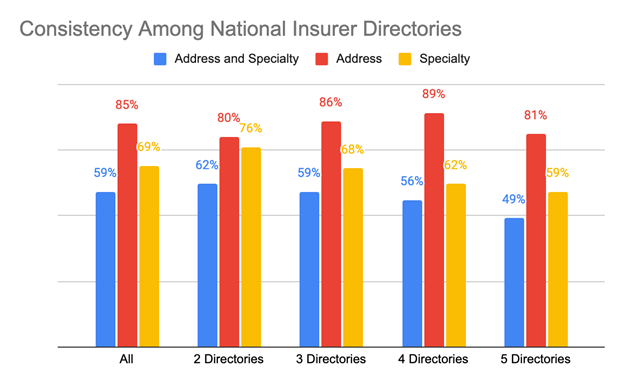
The No Surprises Act prevents surprise bills for out-of-network care and requires insurers to keep updated physician directories. We’re not off to a good start! Researchers searched through online publicly available directories from Elevance (Anthem), Aetna, Cigna, Humana and United Health Care, and of the 635,000 physicians, 449,000 were in at least two directories. Here’s how (in)consistent the data about addresses and specialty was
Source: Butala, et al JAMA March 14, 2023 LINK
Addresses were more likely than specialty to be consistent across directories, but generally 4-5 in 10 physicians had inconsistent address or specialty information across different national health plans. These researchers say they didn’t flag differences in suite numbers or abbreviations, and they assessed only consistency, not accuracy. Some of these inconsistencies were likely to be of little practical importance, and the researchers were not able to assess other salient issues such as whether physicians were accepting new patients.
Implications for employers:
- Members are likely to face inaccurate information in provider directories
- The No Surprises Act holds group health plans (sponsoring employers) responsible for accurately informing members of in-plan status, and accurately attributing payments to in- or out-of-network deductibles.
- Employers should continue to hold health plans accountable for offering members accurate and up-to-date provider information data in member directories.
4. Poll shows steep increase in Americans reporting they are delaying necessary medical care
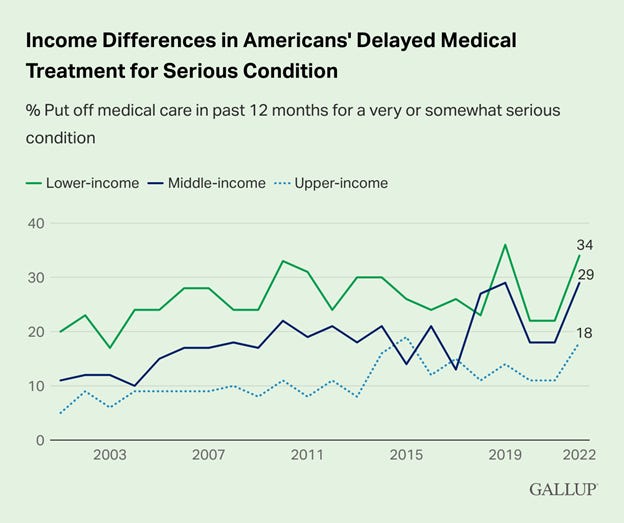
Gallup reported that a record-high portion of Americans (38%) reported that they or a family member put off health care in 2022, up from 26% in 2021. Seventy one percent of those who reported delayed care said this was for a very or somewhat serious condition. Those earning under $40,000 annually were almost twice as likely to report delay of care for a serious condition than those with annual income of over $100,000.
Source: Brenan, B Gallup January, 2023 LINK
Those under 50 were most likely to report delay of care for a serious condition, while those over 65 were least likely to report such a delay.
Source: Brenan, B Gallup January, 2023 LINK
Implications for employers:
- Health care affordability remains a substantial challenge
- This challenge will increase with the end of the pandemic emergency, which has already led to cuts in SNAP (Supplemental Nutrition Assistance Program, previously called food stamps) and will lead millions, including some eligible for employer-sponsored health insurance, to lose Medicaid eligibility.
- Employers can ease this burden somewhat through premiums indexed to income, and by offering health insurance plans with lower point-of-service costs.
- Here’s a link to a 2019 Harvard Business Review article I coauthored with my colleague Steve Nyce and I wrote about health care affordability for low wage workers in.
Brief Followup:
Novo Nordisk and Sanofi each announced this week that they will follow the lead of Eli Lilly and substantially reduce the prices of their insulin products, too. These three companies represent most insulin sales in the United States. This is good news for both employers and health plan members, although the Sanofi and Novo price cuts are not effective until January, 2024. Novo is not offering an out-of-pocket cap, and the Lilly price cuts are effective at various points in 2023.
Hope all have a great weekend when it comes.
Jeff