Claims analysis shows impact of increased use of GLP-1s
June 9, 2025
Summary: Researchers described a large increase in use of GLP-1s for obesity and a decrease in bariatric surgery from 2019-2024. They described an increase in potential complications, but did not report on whether there was a decrease in cardiovascular events.
Source: Fair Health, May 27, 2025
Fair Health, a nonprofit that obtains de-identified claims from multiple health plans, analyzed its 51 billion claims to assess the impact of GLP-1s. The organization does not have medical records, so its reporting is limited to what clinicians put into medical claims. Fair Health also does not know the member’s plan design, so the denominator in this study includes all patients, including those whose insurance does not offer coverage for GLP-1s to treat obesity. Fair Health could have underestimated use of GLP-1s because these medical claims would not have included self-paid or compounded medications.
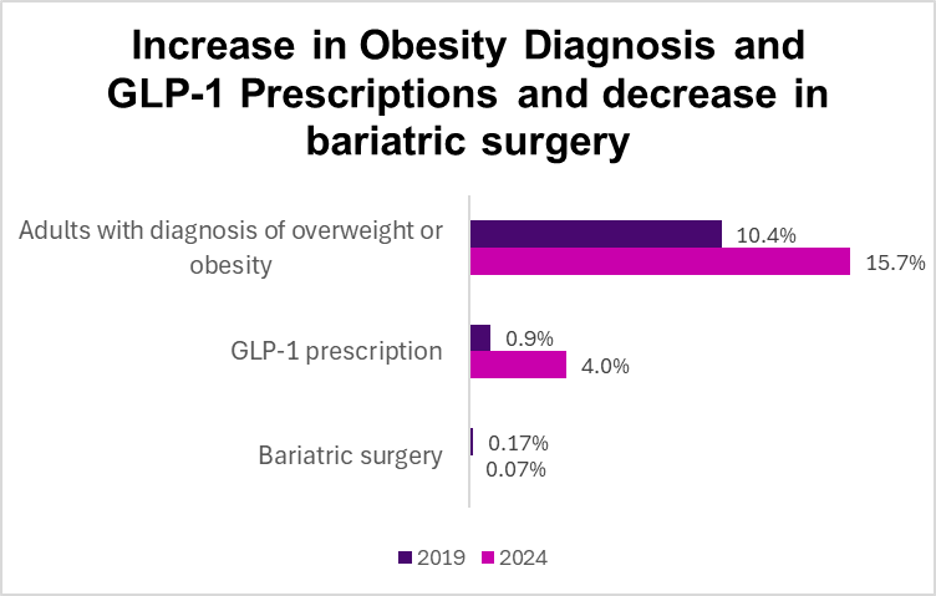
Fair Health reports that the portion of adults with a diagnosis of obesity went up by 51%, from 10.7% to 15.7%. This doesn’t necessarily mean that more adults became obese but could mean that more physicians coded obesity as a billing diagnosis to justify prescribing GLP-1s. The researchers reported that 4% of all adults had been prescribed a GLP-1 medication for either diabetes or obesity, and 2% of all adults were prescribed a GLP-1 medication specifically for obesity.
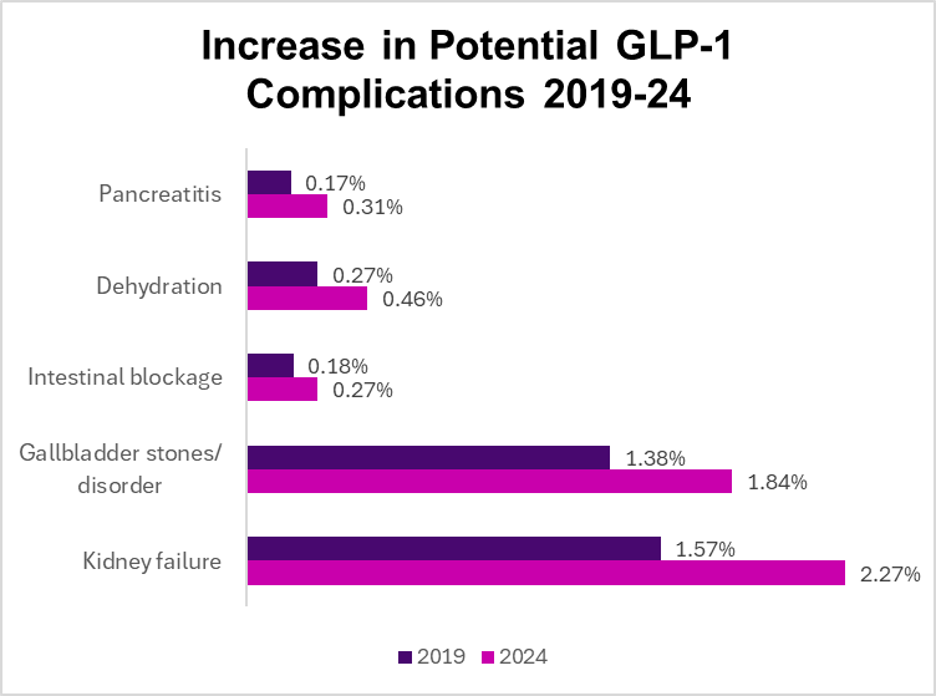
The researchers also reported a higher number of medical claims for many conditions that can be exacerbated by GLP-1 medications, including gallbladder problems, pancreas inflammation, and intestinal blockage. The increase in these diagnoses might have been due to factors other than the increase in GLP-1 prescriptions. The researchers did not report on changes in rates of cardiovascular events.
Source: Fair Health, May 27, 2025
Fair Health reported that in 2024, 40% fewer people had bariatric surgery compared to 2019. Few of those who had bariatric surgery were prescribed GLP-1s afterward (rounded to 0%).
Implications for employers:
The demand for GLP-1 medications for both diabetes and obesity continues to increase.
GLP-1 drugs might be responsible for an increase in some serious adverse events, although the researchers did not capture any potential benefit of GLP-1s, i.e. a decrease in cardiovascular events. Other studies have shown a decrease in heart attacks and strokes by year two of therapy.
Bariatric surgery has a long track record of safety and effectiveness, and is more cost- effective than GLP-1 medications to treat obesity. But clearly a once-a-week injection is more attractive to many seeking obesity treatment.
Thanks for reading! Hope you’ll subscribe to this newsletter, and please hit the "like" button. Please also recommend to friends and colleagues - it's free. You can find previous posts at this link.
Views expressed in Employer Coverage are purely my own.

Recent data suggest GLP-1s may alter gut microbiota diversity, influencing metabolism beyond weight loss. Additionally, real-world cardiovascular benefits might emerge after prolonged use beyond current claim analyses.