I took a week off, and this week am republishing slightly revised posts from the past year. I’ll return with new posts on Monday.
Summary: Colorectal cancer screening has been responsible for a substantial decline in deaths from colorectal cancer. Screening with FIT tests is almost as effective as colonoscopies for those at average risk but much less expensive.
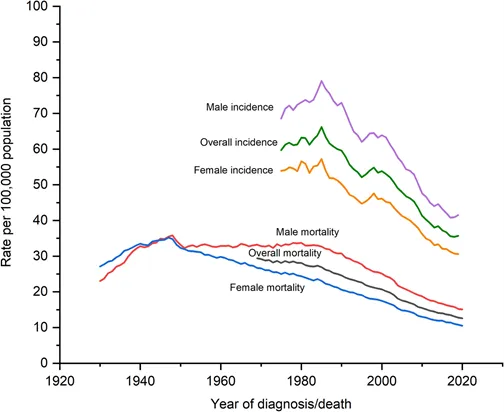
Colorectal cancer deaths, 1930-2020
Source: Siegel, et al 2023. Incidence data is from 1930-2020, and mortality data is from 1976-2019, and is calculated from the SEER (Surveillance, Epidemiology, and End Results) database. LINK
Colorectal cancer death rates have plummeted in the last two decades, largely because colonoscopies identify and remove many polyps which would otherwise have turned into cancers. About 150,000 new cases of colorectal cancer will be diagnosed this year, and there will be about 50,000 deaths. Over half the new cases of colorectal cancer are in those people over age 65, but a third are in those between 50 and 64 years of age, and one in eight new cases are in those under 50 years old.
The USPSTF now recommends regular colorectal cancer screening for those ages 45 and over. Despite that recommendation, national rates of colorectal cancer screening is just over 55% for the commercial PPO population.
The Affordable Care Act requires that this screening is covered without out-of-pocket costs by employer-sponsored health insurance. Still, some who have colonoscopies find themselves with out-of-pocket expenses for some component of the screening (such as lab tests or anesthesia). Colonoscopies for those with symptoms like bleeding or to follow up on a previous polyp are considered “diagnostic,” and members can be responsible for deductible, copay and coinsurance. Surprisingly, patient costs for “diagnostic” colonoscopies are a common complaint to HR teams and insurers.
The USPSTF recommends screening via any one of a number of methods, each of which has advantages and disadvantages. As you can see, many colorectal cancer deaths can be prevented by any of the screening methods. It’s most important that people are screened, whichever screening method they find most acceptable.
Source: USPSTF 2021 LINK Data for screening those ages 45-70
Source: USPSTF, approximate prices from Health Care Blue Book (prices vary by location)
Source: Imperiale, et al NEJM March 14, 2024 LINK These are results of screening colonoscopies performed on over 20,176 patients.
New England Journal of Medicine published research comparing results of a newer version of the Cologuard test with the FIT test. This version of the genetic test, which requires the patient to send a sample of stool by mail, was statistically significantly more sensitive (missed fewer cancers diagnosed by colonoscopy) but was less specific (had a higher number of false positives).
A positive FIT test or stool genetic test requires workup with a colonoscopy to remove polyps or biopsy any potential cancer. The FIT test, if done instead of a colonoscopy, should be repeated each year, while stool genetic tests are generally repeated every three years. Therefore, over a multi-year period the sensitivity of FIT tests in clinical practice will be higher than in this study (and the specificity will be lower).
Many find the prep for colonoscopy especially difficult. Here’s one way to make the prep more acceptable: a gastroenterologist wrote in StatNews this week that low residue diets (such as eggs, white bread, pasta and cheese) are just as effective as liquid-only diets the day before colonoscopy.
Implications for employers:
Colorectal cancer screening saves lives, and too many people are not being screened.
The “gold standard” for those at average risk of colorectal cancer from ages 45 to 75 is a colonoscopy every 10 years.
Employers can ask their carriers to report their colorectal cancer screening rates using a denominator of who is eligible for screening.
Those who have had polyps in the past often must pay deductible or cost sharing payments for future screening colonoscopies. Employers can ask their carriers to cover all screening colonoscopies as preventive care without cost sharing. Recent research even suggests this can be cost saving.
This note originally published in March, 2024 for Colorectal Cancer Screening Awareness Month.