Friday Shorts: Flu, NIH cuts, gene therapy companies in trouble, GLP-1s and obesity
February 28, 2025
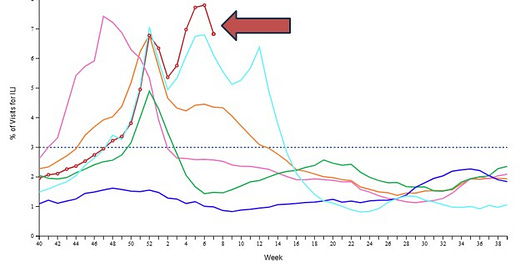
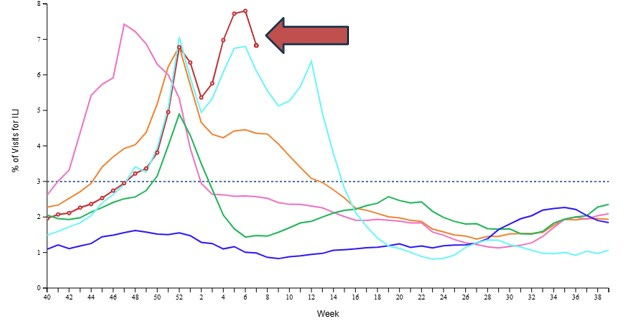
A) Influenza rates continue to be high across the country
Source: CDC, week ending February 15, 2025. This chart shows the portion of adult visits for influenza-like illness, which remains higher than any recent year. The rate is finally down a bit from the previous week.
This is the first season since the COVID pandemic that deaths from influenza have exceeded deaths from COVID-19. There have been 68 confirmed deaths of children from influenza this season.
I recommend this New York Times article by Caitlin Rivers pointing out that “most people want their shots.” Gift Link
B) CRISPR (gene editing) companies are in financial trouble
Gene editing company stock price change since January 1, 2021
Source: Mast, J StatNews, February 6, 2025
StatNews reports that the companies that are using gene editing to create drugs that can cure genetic diseases are in deep financial trouble. Their drugs are so expensive when they make it to market that they are rarely used. As a result, these companies are finding it difficult to recruit investors to cover the costs of the expensive clinical trials necessary to gain FDA approval.
Apparently, fewer people have been treated with the new sickle cell disease genetic therapies since they were approved in 2023 than participated in the pre-approval trials. (Casgevy was infused in 40 people since commercialization after being tested in 44 people in clinical trials. Lyfgenia was infused in 25 people since its approval after 65 participated in clinical trials).
BluebirdBio, the maker of Lyfgenia, just agreed to sell itself to private equity for $29 million, approximately the revenue of under a dozen treated patients. The company’s peak valuation since it went public was $10 billion.
The next generation of genetic therapy will hopefully not require major chemotherapy to quell the immune system and might gain more uptake. Gene editing continues to have the promise to cure many genetic diseases, but without commercial success these therapies will not become available.
C) National Institute of Medicine cuts
Although cuts in NIH are currently on hold due to judicial injunctions, the New York Times reports that the NIH has distributed $1 billion less as of mid-February in 2025 compared to last year. Here’s a link to a compelling StatNews story written by a pediatrician whose sister died of a rare disease that was treated at the NIH. StatNews reports that universities and medical schools have withdrawn or frozen new graduate school admissions. Here’s a link to NPR’s Planet Money podcast on the impact of these cuts.
D) Recently trained clinicians more likely to prescribe GLP-1 medications
Portion of physicians who prescribed a GLP-1 medication for diabetes
Source: Inoue, J Gen Int Med January 22, 2025
The Journal of General Internal Medicine reports that physicians less than 10 years out of training are more likely to prescribe GLP-1 drugs for diabetes than physicians out of training for longer. Given that the GLP-1 drugs (and another newer category of medications for diabetes, SGLT-2 drugs, such as Jardiance) are very effective at preventing heart and kidney disease, it’s disappointing to see older physicians have slower adoption. This study did not include advanced practice clinicians (PAs and NPs) and might have included many physicians who do not provide direct care for patients with diabetes.
E) GLP-1s decrease COPD exacerbations
A new study in JAMA Internal Medicine shows that those with diabetes and chronic obstructive pulmonary disease were less likely to be hospitalized when treated with either GLP-1s or another newer class of diabetes medicines, SGLT2s (such as Jardiance). This was a large study of claims from multiple sources, although the researchers did not have access to income levels of the patients. Those who have both diabetes and COPD have better outcomes when treated with these newer (and more expensive) drugs.
F) Non-medical intervention was effective for pediatric obesity
Pediatrics reported that a group of 270 predominantly Black and Hispanic children ages 5-17 participating in a program that paired clinical obesity care and group-based lifestyle sessions at a local recreation center had statistically significant weight loss compared to a randomized control group. The cost of the program was very low ($150 per child for the year) so this could be scalable. Here’s a summary from the Washington Post.