Gastrointestinal side effects of anti-obesity medications
May 13, 2024
Source: Bartelt, et al Epic Research Network May 1, 2024 LINK
A few recent publications give us some additional data about expected side effects from the GLP-1 anti-obesity medications. In a study of 12 million people with diabetes (4.6 million on GLP-1 medications and 7.4 million on other medications), researchers found substantially more delayed gastric emptying with the GLP-1 medications that were in use earlier, which are generally not used for obesity. This study did not find higher rates of gallstones, often associated with weight loss, with these drugs, and found fewer episodes of ileus, or blocked colon, than expected based on age and other medical conditions.
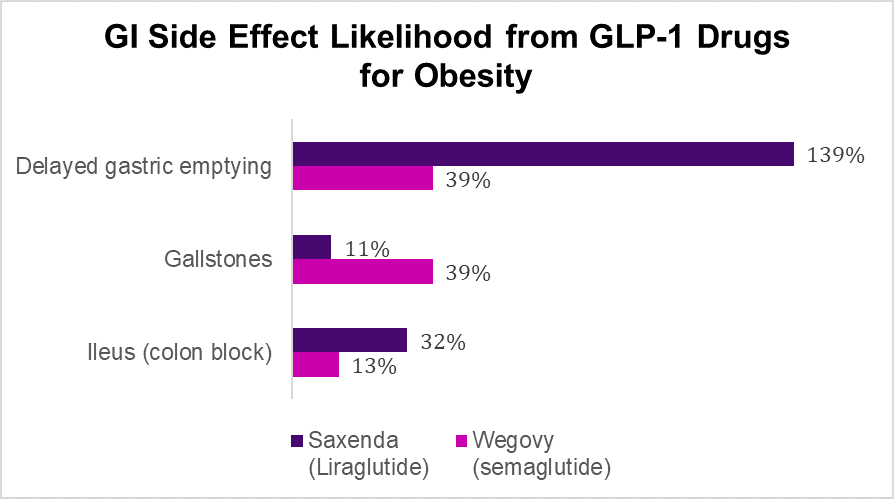
In a parallel study of those on weight loss medicines, researchers compared about 171,000 who were on GLP-1 medications with about 197,000 who were on other weight loss drugs, and found that liraglutide (Saxenda) more than doubled the incidence of delayed gastric emptying, and that semaglutide (Wegovy) increased this side effect by more than a third (39%) compared to non-GLP-1 drugs. Delayed gastric emptying is one of the mechanisms by which the GLP-1 medications decrease appetite. Tirzepatide (Zepbound) was not included as that drug was only approved for obesity late in 2023. Semaglutide also increased the rate of gallstones by more than a third (39%), though liraglutide did not.
Source: Bartelt, et al Epic Research Network May 2, 2024 LINK
In an unrelated study published in JAMA last month, researchers compared anesthesia complications from about 3,500 people with diabetes on GLP-1 medications with anesthesia complications of about 20,000 people with diabetes treated with other medications. The researchers only included patients who had operations the same day they were seen in an emergency department. People on GLP1s who had emergency surgery (without time to tell them to stay off their GLP1s for a week to avoid trouble with anesthesia induction due to a full stomach) had no more anesthesia complications than a control group on other anti-obesity drugs.
Implications for employers:
GLP-1 medications can cause GI problems and that is why starting doses are gradually increased. A minority of patients cannot tolerate the GI symptoms and will need to stop the GLP-1 altogether.
The drugs have different profiles – so a patient who has GI symptoms on one drug might tolerate a different drug in the class.
Those with diabetes and those with obesity might have a different risk profile for these complications.
These drugs have known benefits, namely they reduce (1) weight, (2) risk of diabetes, (3) progression of renal disease, (4) major adverse cardiovascular outcomes; but these benefits come with tradeoffs.
Not everyone who is eligible for GLP1s will choose to be on them. Some who take them won’t achieve > 5% weight loss, and others will find the side effects intolerable. So, there is still a role for other programs to help people lose or stop gaining weight.
Bariatric surgery is effective and more cost-effective than GLP-1 medications.
Thanks for reading. You can find previous posts in the Employer Coverage archive
Please subscribe, “like” and suggest this newsletter to friends and colleagues. Thanks!
Tuesday: Retailers retreating from primary care