Cardiovascular disease mortality rates, 1980-current
Source: Martin, et al Circulation February, 2024
When I was in training in the mid-1980s, I saw a young patient almost every week (almost always a smoking man between 45-55) in the Coronary Care Unit with a life-changing or life-ending heart attack. Much has improved since then. Adult smoking rates are about a third of what they were, powerful statins can lower cholesterol, and well-tolerated medicines control blood pressure. Statins and blood pressure medicines are also generic and unimaginably cheap.
Our medical interventions have improved, too. Stents, tiny spring-like devices, keep coronary arteries open after an angioplasty to treat plaque inside arteries that can cause a heart attack, and blood thinners increase success rate. Fewer people need coronary artery bypass grafts for heart disease. Excellent drugs are available to treat diabetes and obesity.
Heart disease rates went down in the U.S. from 1980-2010, but they’ve been on the upswing since then as seen on the chart above. It’s disappointing that the decrease in smoking and the improvement in medical treatments has not led to continuing improvement in cardiovascular disease.
Cardiovascular hospitalization rates U.S. and Denmark
Source: Berg, et al JAMA Cardiology February 5, 2025
A study published last week in JAMA Cardiology demonstrates that among adults over age 65, the rate of hospitalization for cardiovascular disease is 50% higher in the U.S. than in Denmark. Risk of congestive heart failure is 2.4 times as high in the U.S., although the Danes have a 10% higher rate of stroke.
This is a large study, assessing outcomes in over 56 million Americans and almost 1.2 million Danes. Although this study is among senior citizens, behavior and medical care before age 65 weighs heavily in increasing cardiovascular risk. A substantial reason for this increased risk is the higher rate of hospitalization in the U.S. among those with lower incomes (see below).
There are non-clinical factors which may have impacted these results, including how these conditions are coded and the criteria for hospitalizations in each of the countries.
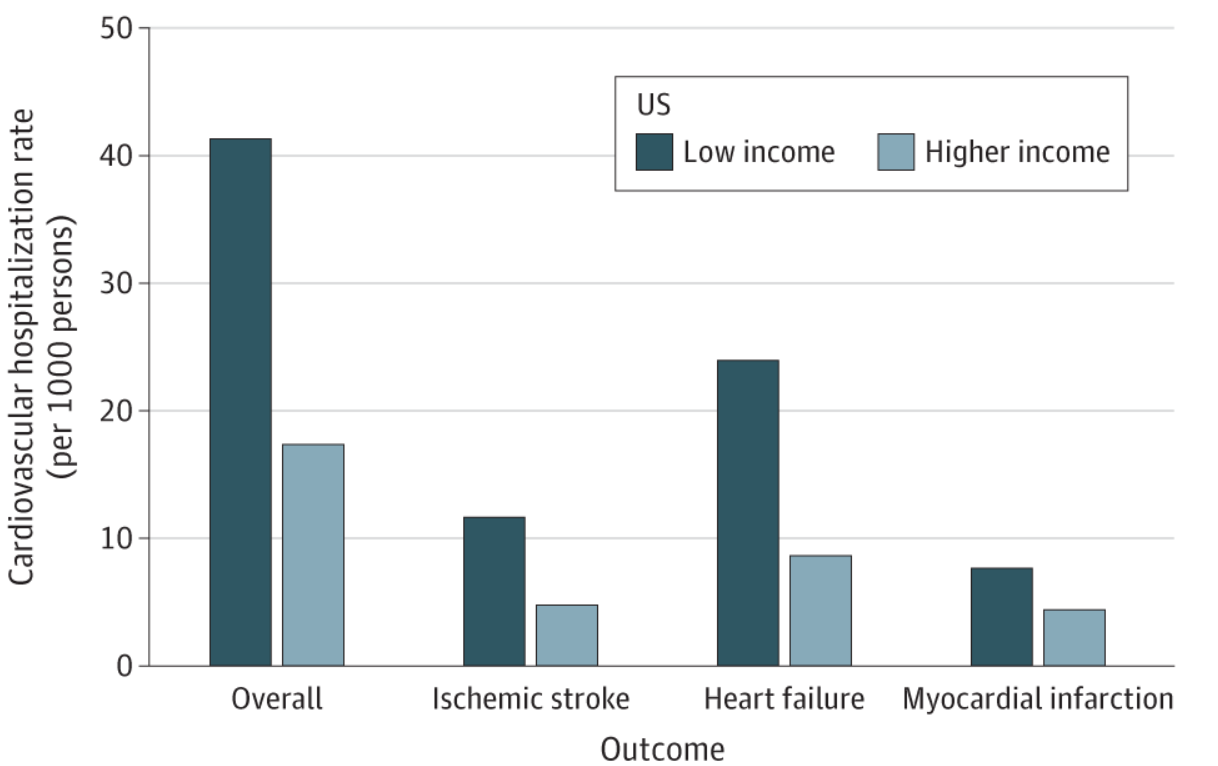
Cardiovascular Hospitalizations in U.S. by Income
Source: Berg, et al JAMA Cardiology February 5, 2025.
Low income was the bottom 15% of income, and high income was everyone else. Those with disabilities may have been overrepresented since dual Medicare-Medicaid eligibility determined “low income” status.
Implications for employers:
There is a large opportunity to decrease illness and death from heart disease in the U.S.
Cardiovascular risk can be lowered by decreasing smoking rates, improving treatment of metabolic syndrome, high blood pressure, high cholesterol and diabetes.
Treating obesity effectively can also lower the risk of major cardiovascular events. Studies have already shown that bariatric surgery and GLP-1 medications decrease major cardiovascular events.
Employers can continue to support smoking cessation and can include metrics around decreasing cardiovascular risk in their carrier performance guarantees.
Tomorrow: Cuts in NIH “indirect” funding could have substantial impact on hospitals and research