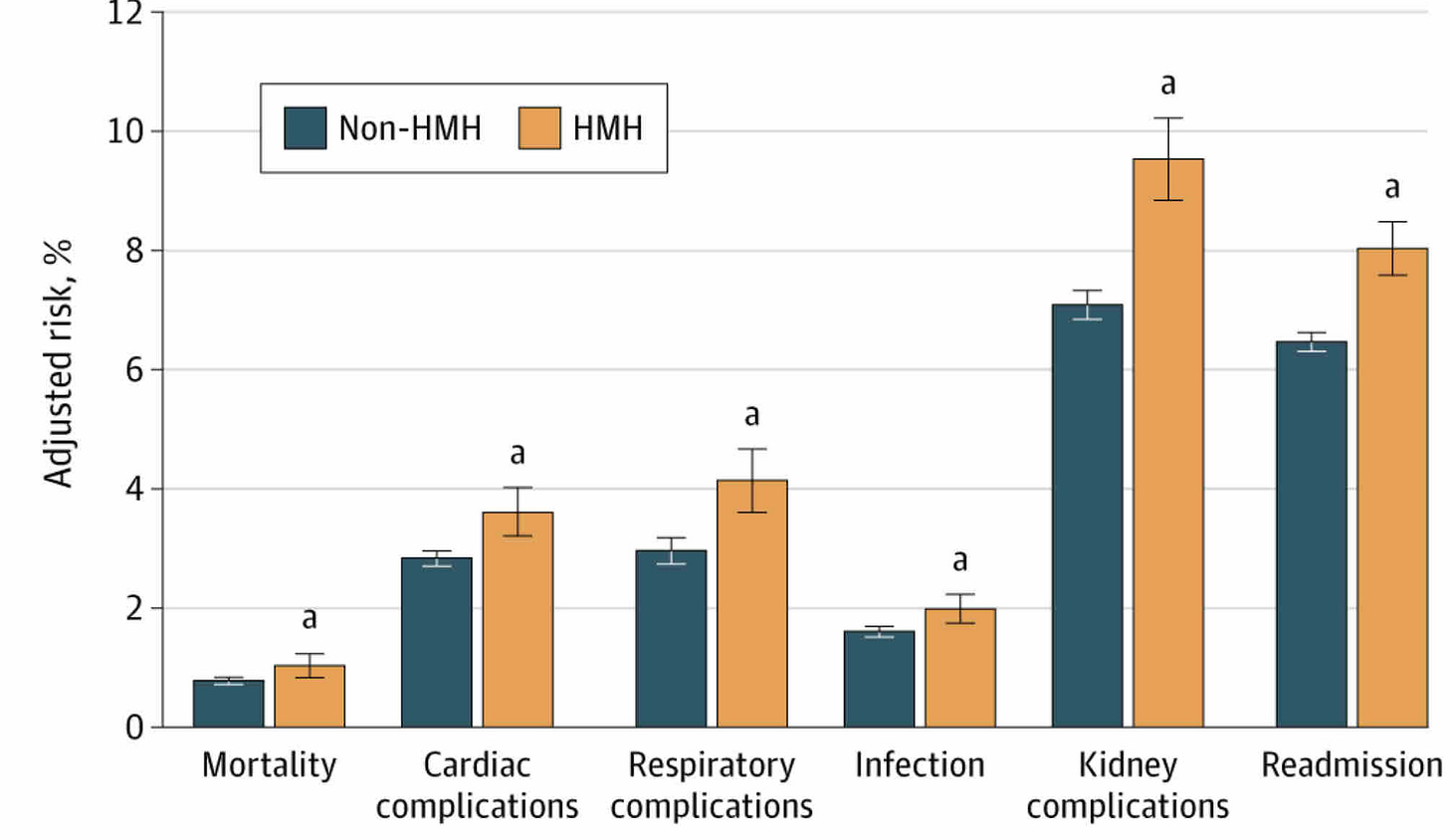
Summary: Hospitals with higher markups had statistically significantly worse surgical outcomes.
Adjusted risk of adverse outcomes based on hospital markups
Source: Sakowitz, et al JAMA Surgery, September 24, 2025. “a” indicates a statistically significant difference. HMH = a high markup hospital)
Research published in JAMA Surgery shows that hospitals which have list prices that are especially high compared to their cost of care have poorer surgical outcomes. The researchers examined Medicare cost reports to assess the markup of each of almost 2000 hospitals. Those that had markups in the top 10% were considered “high margin hospitals,” and had median markups of 8.5x. Median markups of the all hospitals evaluated was 3.5% The high margin hospitals were more likely to be for-profit hospitals in metropolitan areas, and took care of a larger portion of Medicare beneficiaries.
The markups reflect the hospitals’ chargemaster -not the actual amount collected from patients or payers. In fact, discounts at U.S. hospitals for commercial health plans are often close to 50%, and discounts for Medicare and Medicaid are higher. Further, hospitals might offset losses on other services through making profits on these procedures. Hospitals with high markups don’t necessarily have the highest prices.
The researchers evaluated the outcomes for over 367,000 care episodes for four major elective surgeries: abdominal aortic aneurysm repair, colectomy, coronary artery bypass grafting, and hip replacement. They found a statistically significantly higher rate of complications in those getting these surgeries at high markup hospitals, including more heart, lung and kidney complications, more infections and more readmissions.
This finding is an association - and doesn’t prove causality.
Implications for employers:
There are substantial differences in outcomes among different hospitals, and those hospitals which have higher markups tend to have worse surgical outcomes.
This supports efforts to use centers of excellence or narrow networks to steer patients to higher value providers.
This research points to the challenge of evaluating payers or providers based on percentage discount. Actual costs rather than discount rates are now more available due to transparency in coverage regulations.

I love the information you share...keep up the solid effort