Summary: Over the entire population, the rate of death from cervical cancer has declined substantially since HPV vaccination began in 2006.
Just in time for Thanksgiving, JAMA published a summary of the striking decrease in deaths from cervical cancer among young women that began around 2015, when the first cohort of young women were protected by the human papilloma virus (HPV) vaccine. Cervical cancer deaths had been declining by about 3.7% a year from 1992-2015, and they decreased about 15.2% per year from 2015-2021.
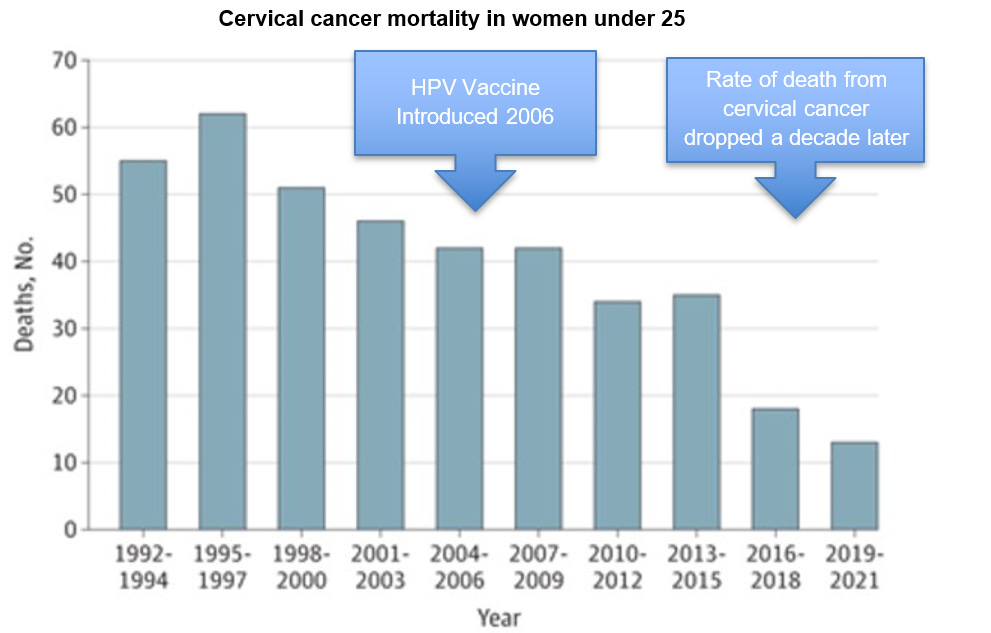
The first graphic shows the decline in death rate.
Source: Dorali, et al JAMA November 27, 2024. This shows that the rate of cervical cancer deaths dropped more rapidly starting ten years after introduction of the HPV vaccine.
The second graphic shows that the rate of cervical cancer death was already decreasing, likely due to screening and improved treatment of invasive disease. This decline increased dramatically from 2015 on, associated with the first cohort to have been protected by the HPV vaccination. HPV virus also causes throat and head and neck cancers, although we will not have data on impact on population mortality for decades.
Cervical cancer mortality in women under 25
Source: Dorali, et al JAMA November 27, 2024
The Centers for Disease Control and Prevention (CDC) reports that 76% of young women had at least one dose of HPV vaccine, and 62.6% were up to date (3 vaccinations) in 2022. Previous research demonstrated that the HPV vaccine was associated with an 86% decline in cervical cancer if administered between ages 14-16, and no cases of cervical cancer in those who were vaccinated before age 14. The HPV vaccine is currently recommended for adolescent boys and girls and has been shown to be safe. There is no evidence that young teens who are vaccinated are more likely to engage in earlier sexual activity.
Implications for employers:
- This is an example of where a childhood vaccine can prevent cancer and cancer deaths.
- The HPV vaccine will likely also prevent many cases of throat and related cancers in middle aged adults, although studies demonstrating this will take decades.
- The HPV vaccine is recommended by the Advisory Committee on Immunization Practices, and is available without cost sharing to those with employer-sponsored health insurance.
- Employers can request their carriers report on HPV vaccination rates and can provide educational material to encourage their members to get their children vaccinated.