Insulin “rationing,” new guidelines for transgender coverage, worsening maternal mortality rate, and COVID-19 roundup
October 21, 2022
Insulin “rationing,” new guidelines for transgender coverage, worsening maternal mortality rate, and COVID-19 roundup.
Today, I’ll cover a new study showing that many diabetics take less insulin than recommended to save money, a new article by a colleague summarizing new standards of coverage for transgender care, two new reports from the Government Accountability Office (GAO) on maternity care in the US, and provide a brief COVID-19 roundup
1. Insulin “rationing” common even among those with employer sponsored health insurance
The Annals of Internal Medicine published data from the 2021 National Health Interview Survey which found that 16.5% of respondents reported that they took lower doses of insulin than recommended due to financial concerns. Insulin rationing was less common in those over age 65 (11.2% vs. 20.4% in those under 65). Of those who were privately insured, 18.8% reported that they skipped insulin doses, took less insulin, or delayed buying insulin to save money.
Skipping insulin or taking too low a dose is life-threatening for those with Type 1 diabetes, and can cause premature vascular disease, kidney failure, and blindness in those with Type 2 diabetes. The Inflation Reduction Act required copays of $35 or less for insulin for those on Medicare, but a federal requirement that private employers put such a ceiling on insulin costs was defeated in the Senate.
Many diabetics are on multiple medications, and newer brand-name drugs, which are clinically much better for most patients than older diabetes drugs, often cost even more than insulin. For those on insulin, the cost of test strips or continuous glucose monitors can also be very high – adding to the crisis of affordability. The nonprofit Civica Rx and the State of California have both announced plans to produce and sell biosimilar insulin for around $30 a vial, although we don’t yet know if this will be on PBM formularies.
Implications for employers:
- Many employers already use a “value based formulary” where insulin and other diabetes medicines are offered without cost share. The Internal Revenue Service clarified in 2019 that employers can offer first dollar coverage for diabetes medications in High Deductible Health Plans with tax-advantaged Health Savings Accounts.
- Value based insurance design can insulate diabetics from the high cost of insulin or other lifesaving drugs, but we cannot lose sight of the underlying problem of the high acquisition cost of these drugs.
- Some diabetes vendor solutions provide access to diabetic supplies without out-of-pocket cost, which can increase adherence to testing recommendations.
2. WPATH introduces new standards for coverage of transgender care
WPATH (the World Professional Association for Transgender Health) released its new Standards of Care in mid-September, and there are substantial changes from the previous version published a decade old. My WTW colleague Patricia Toro, MD MPH did an excellent review of implications for employers published this week in Human Resources Executive. Changes include more inclusive language, a move away from requiring a mental health diagnosis (gender dysphoria) for treatment, and more flexibility about when and which gender affirmation procedures should be covered. The Human Resources Campaign has not yet incorporated these recommendations in its Corporate Equality Index.
Implications for employers:
- Employers can review these new guidelines as they consider how to offer inclusive benefits.
3. U.S. maternity care worsened in the pandemic, and COVID-19 vaccination associated with better pregnancy outcomes
The Government Accountability Office (GAO) released two reports this week about maternity care in the United States. The first demonstrates worsening maternal mortality due to the pandemic. For the first time in recent years, more than 1000 women died of pregnancy related causes in 2021, and about a quarter of these were directly due to COVID-19. Black maternal mortality was 44 per 100,000 births in 2019, and rose to 69 per 100,000 births in 2021.
Source: GAO October 18, 2022 LINK
The second GAO report confirms that obstetric access in rural areas is getting worse. Half of rural counties don’t have a hospital with maternity services, and the problem is worse in rural areas with lower incomes and more minority residents. This confirms reporting from the March of Dimes earlier this month that I mentioned in last week’s note.
Meanwhile, JAMA Pediatrics published research this month that demonstrated that COVID-19 vaccination in pregnancy was associated with lower risk of neonatal intensive care unit admission and fetal death, and was not associated with any adverse pregnancy outcomes. About a third of pregnant women in the U.S. have not been fully vaccinated against COVID-19.
Implications for Employers:
- Employers pay for a bit over half of all deliveries in the United States, and can encourage their health plans to provide adequate information on maternity services to their members, and to contractually require quality reporting by delivery services.
- Employers can continue to encourage COVID-19 vaccination and boosting.
4. COVID Roundup:
a) Vaccination and boosting leads to less COVID-19 illness
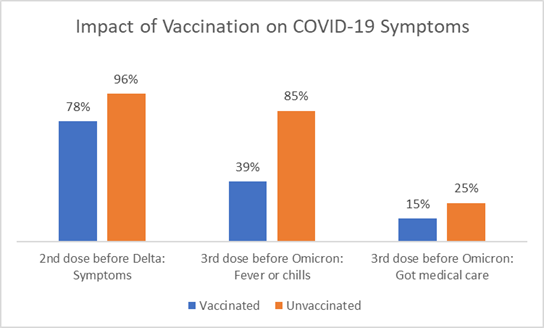
Researchers in JAMA Network Open reported on about 1200 frontline and essential workers who were infected with COVID-19 through early 2022, and found that those who had more vaccinations had fewer symptoms and lower viral loads than those who had fewer vaccinations.
Source: JAMA Network Open, October 18, 2022 LINK
b)New variants on the way.
The variant that dominates infections seems to change a few times a year, and we can often look to Western Europe to gauge what to expect in the coming weeks. In the US, BA.5 remains dominant (68% but decreasing), and BA.4.6 is the second most common strain at 12% (unchanged). BQ.1 and BQ.1.1 are also at about 11% and increasing; these strains are even more frequent in the Northeast, and have been growing rapidly in Western Europe. The BQQ variant, which is causing an uptick in cases in Singapore and East Asia, still represents few cases of COVID-19 in the US.
c) New bivalent booster likely to be effective against new variants
Both BQ.1 and BQ.1.1 are descended from BA.5 - which is good news for vaccination. The FDA instructed Moderna and Pfizer to produce a bivalent vaccine targeted to the BA4/5 spike protein, which will hopefully mean better protection against these new variants. The UK and other European countries used a bivalent booster based on the BA.1 variant, which is less similar.
Vaccines only work if they are used! About 14.8 million Americans have received the updated booster as of October 19.
d. New variants likely to overcome immunity from monoclonal antibodies
The news isn’t as good for monoclonal antibodies, though. Evusheld, used for 6 months of protection for the immune compromised, is apparently much less effective against BA.1 and BA.1.1, and there is unfortunately not yet a good alternative.
e. Novavax booster approved
The FDA approved the Novavax vaccine as a booster shot for those who are unable or unwilling to take either the Moderna or Pfizer mRNA vaccine. This is only relevant for those who need a first booster - and was designed for the original virus strain, so is likely less effective against the newer variants than the bivalent booster.
f. Life expectancy in the U.S. continued to decline in 2021
Researchers in Nature Behavior reported that we lost 2.7 months of life expectancy in 2021, in addition to the 25.5 months of life expectancy lost in 2020. Many western Europeans saw life expectancy start to recover in 2021, although only Norway had life expectancy in 2021 that exceeded that in 2019. Vaccination rate was strongly correlated to improvements in life expectancy by country and age. Of special interest to employers, more than half of the lost life expectancy was in people under age 60.
(I intended to post this on 10/21 - but must have missed a step. Next post is on 10/28.)