Summary: Women with early stage cervical cancers did not receive additional benefit from more invasive surgical procedures.
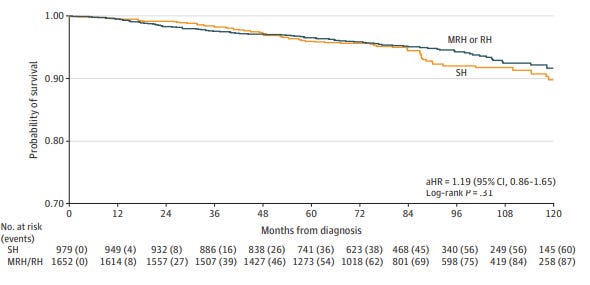
Adjusted survival estimates
Source: Tarney, CM et al JAMA Network Open May 15, 2025. SH= “simple” hysterectomy; MRH or RH = modified radical hysterectomy or radical hysterectomy. The difference in mortality at 120 months) does not reach clinical significance.
There are about 11,500 new cases of cervical cancer diagnosed and about 4,000 women die of cervical cancer each year in the U.S. A new study in JAMA Network Open evaluated outcomes among 2636 women with early stage cervical cancer treated at National Comprehensive Cancer Centers. They found that survival rates and complications were similar in women who received a simple hysterectomy (removal of the womb with or without removal of ovaries and fallopian tubes) compared to those who had a radical hysterectomy (removal of womb, ovaries, fallopian tubes, nearby lymph nodes and a portion of the vagina). The women were initially diagnosed between 2010 and 2017, and found to have similar 3, 5, 7 and 10-year survival rates, and did not have higher rates of recurrence or require significantly more radiation or chemotherapy treatment.
This is important, because women who have the radical or modified radical hysterectomy are more likely to have postoperative complications, including bleeding, difficulty with urination and bowel function, and worse quality of life.
HPV (human papillomavirus) vaccinations can prevent most cases of cervical cancer and many cases of throat and neck cancers. The U.S. already has seen declines in diagnosis of new cases of cervical cancer since 2015, when the first cohort of young women were vaccinated against HPV.
Implications for employers:
This study demonstrates that many women with early cervical cancer can be treated less invasively.
Surgeons who offer less invasive surgery with equivalent outcomes should be more likely to be in high value networks, and navigators can steer members to such surgeons.
HPV vaccinations are available without cost sharing, and employers can be sure that they are available through both the pharmacy and medical benefit to offer multiple options for families to get their children vaccinated.