National health expenditures, health care affordability, mental health telemedicine, and current state of respiratory viruses
January 13, 2023
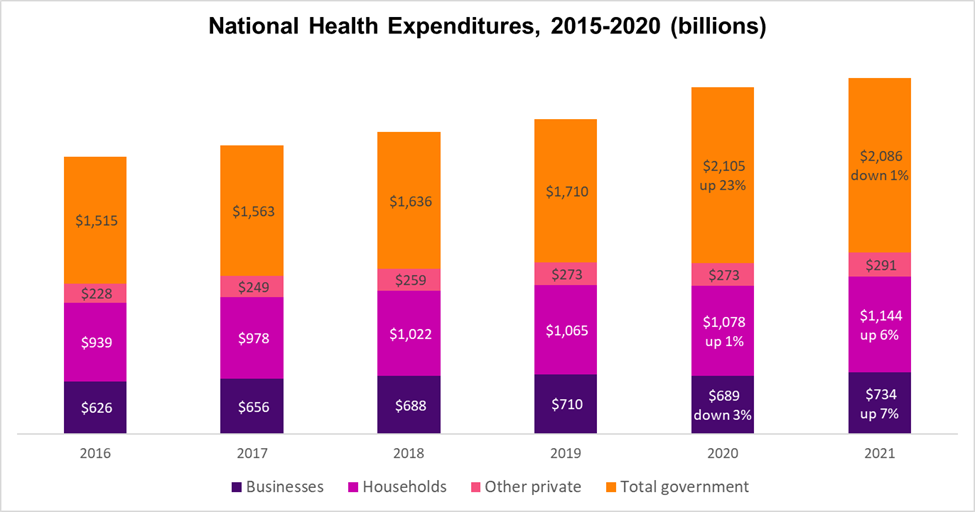
1. 2021 National Medical Expenditures show a big increase in cost for employers and households
Source: Martin, et al Health Affairs, December, 2022 LINK
The CMS Office of the Actuary published its estimate of national health expenditures last month. Government health expenditures costs were up 23% due to pandemic expenses in 2020, compared to 2019, but these costs dropped slightly in 2021. The costs of health care for private businesses went up 7% over the same time period, and the cost of health care for households increased by 6%.
Implications for employers:
- The cost of COVID-19 vaccinations and treatment will transition from government to employer-sponsored health insurance later this year since Congress did not pass additional pandemic funds.
- The unit cost of vaccines and drugs is likely to increase dramatically. Pfizer and Moderna have both announced that COVID-19 vaccinations that the federal government most recently purchased for $26 per dose will cost $110 to $130 each. This is in addition to the cost to administer the vaccines.
- Along with provider consolidation and increased hospital labor costs, these COVID-19 related expenses will likely to lead to continued increases in the cost of employer sponsored health insurance in 2023.
2. Health care affordability remains a challenge for some with employer sponsored health insurance
Researchers reviewed two decades of data from the National Health Interview Survey (NHIS) and showed that affordability initially increased following the implementation of the Affordable Care Act (ACA), but it has decreased since 2016. Reports of inability to afford medical or dental care decreased following implementation of the ACA, but have increased since 2016. The NHIS includes over 230,000 respondents ages 19 to 64. Women report more trouble affording health care than men.
Trends in Reported Inability to Afford Needed Health Care Among
Nonelderly Adults With Employer-Sponsored Insurance, 2000-2020
Source: Gupta, JAMA 12/27/22 LINK
Health Affairs published a study this month demonstrating a correlation between food insecurity and high medical costs in those covered by employer sponsored health insurance. The authors conclude that improving food security could lower health care costs, but I think that in some instances high medical costs and loss of income from illness might be the underlying cause of food insecurity.
Implications for employers:
- Employers can make sure that plan design will not leave necessary medical care out of reach for lower wage workers.
- Here’s an article we published in Harvard Business Review in 2019 reviewing options, which include
- Increased subsidization or cross subsidization, such as having different benefits or premium based on salary
- Offering at least one plan with lower out of pocket costs
- Maximizing outside subsidies
- Narrow high value networks
- Careful review of incentives and subsidies that penalize lower wage workers
- Robust navigation and virtual visits
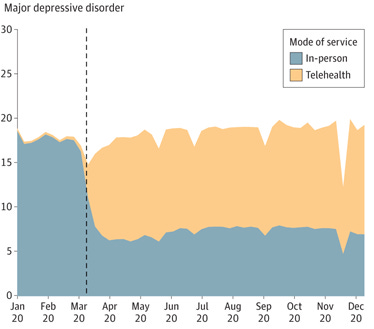
3. Can mental health access gains from telemedicine during the pandemic be sustained?
Mental health care changed dramatically during the pandemic. In-person visits fell by more than half, but the total number of visits were well maintained for most conditions. Here’s data from a study published last week in JAMA Health Forum, showing total visits for major depression in 2020.
Source: McBain, JAMA Health Forum 1/6/23 LINK
There have also been huge benefits in treatment for opioid dependence. Federal regulations removed a cap on how many patients each physician could treat and eased the requirement that those in methadone maintenance programs come to a clinic every day to be observed taking the medication. This meant more could be treated for opioid use disorder, and more under treatment could hold a regular job.
The tele-mental health boom did not come without challenges. Some telemedicine providers are under investigation for overprescribing Attention Deficit and Hyperactivity Disorder (ADHD) drugs, which are highly abusable. Use of these drugs increased enough that there is a nationwide shortage of some types of Adderall in some retail pharmacies, one of the mainstay drugs. And some pharmacies are leery of filling prescriptions from out-of-town telemedicine providers, especially those affiliated with some for-profit startups. And this report from STAT and The Markup article highlighted privacy concerns with some virtual mental health providers.
Implications for employers:
- Employers should continue to offer telemedicine mental health care through their carriers or Employee Assistance Programs (EAPs). Our surveys show that over 90% of employers offer such a benefit.
- The startups that are accused of overprescribing generally sold their services directly to consumers and did not sell their services through employers or bill insurance.
- Reports on mental health utilization should incorporate both in-person and virtual visits.
- Employers should be sure that their virtual mental health providers have good privacy practices in place.
4. Respiratory Viruses: RSV wave has subsided; influenza rising less rapidly; COVID-19 hospitalizations and deaths increasing
As we enter the new year, hospitalization rates for respiratory syncytial virus (RSV), which overloaded pediatric hospitals in the fall, have come back down to levels more usual at this time of year. Influenza hospitalization rates remain high, although they are not rising as rapidly as they were a month ago. Hopefully, the northern hemisphere will not have the second influenza spike seen earlier this year in the southern hemisphere.
COVID-19 rates reported by the Centers for Disease Control and Prevention are no longer accurate since the majority of cases are diagnosed by home test and not reported. Hospitalization and deaths are likely a better indicator of cases these days. COVID-19 hospitalization rates are up 15% over the last two weeks, and there are over 5500 in intensive care units with COVID-19 (as of 1/11/22). Almost 90% of the country has either high or substantial community transmission.
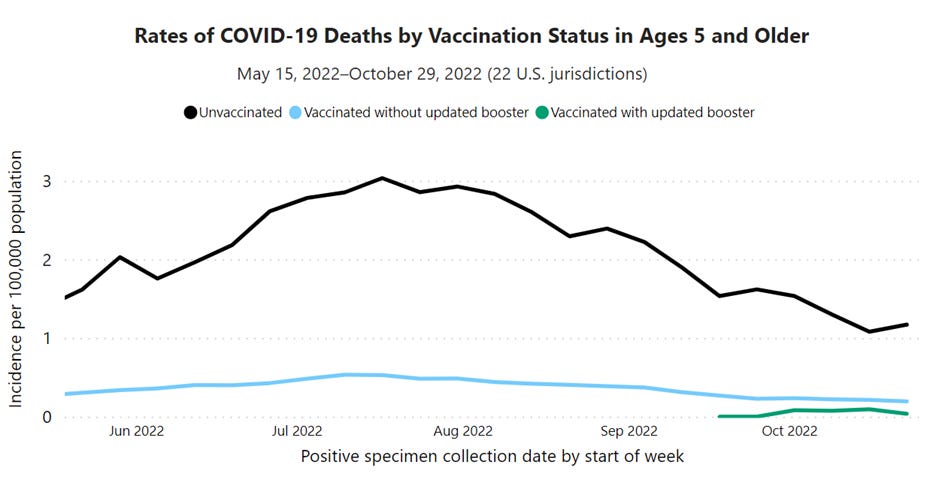
Uptake of the bivalent vaccine, which has been shown to reduce the risk of hospitalization, is only about 15% - so many of these hospitalizations and cases of severe illness are likely preventable. The chart below shows that those who got the updated (bivalent) booster, represented in green, were less than a quarter as likely to die of COVID-19 than those who were vaccinated without the updated booster, represented in blue.
Source: CDC January 11, 2022 LINK
Implications for employers:
- Expect continued high levels of employee absence due to respiratory disease.
- Continue to encourage influenza and COVID-19 vaccinations. It’s not too late to get these vaccines, and they can be given together, usually one in each arm.
- For employees over 50 and for those with compromised immune systems, the drug Paxlovid is associated with fewer hospitalizations, lower mortality, and lower risk of Long COVID.
* * *
Hope you have a wonderful weekend when it comes, and that Martin Luther King Day provides an opportunity to contemplate what we can all do to increase social justice.