New ruling against ACA preventive care coverage, the cost of asthma inhalers, patient empowerment, and air pollution and race.
March 31, 2023
Happy Friday!
In today’s note, I’ll cover two advances in patient-empowerment: patients screening themselves for cervical cancer and gaining access to their laboratory results before their clinicians. I’ll also discuss air pollution’s disparate impact on the health of those who are Black and those who are poor, the high cost of lung disease inhalers even after these medications are off-patent, and a study that demonstrates worse outcomes when patients had preoperative consults to “clear” them for surgery.
But first, some breaking news from Thursday.
A federal judge in Texas ruled that the Affordable Care Act’s requirement that employers cover preventive services recommended by the US Preventive Services Task Force (USPSTF) is unconstitutional and cannot be enforced. That’s because the USPSTF is not appointed by the President and confirmed by the Senate (violating the Appointments Clause of the US Constitution.) This affects the USPSTF recommendations (such as colonoscopies, mammography, and payment for medicine to prevent HIV transmission. This ruling does not affect requirements to cover vaccinations, which are made by the Advisory Committee on Immunization Practices and endorsed by the CDC director. This also does not affect women’s health services such as contraception, as they are recommended by the Health Resources and Services Administration and endorsed by the Secretary of Health and Human Services. Separately, this judge has ruled that religious organizations are not subject to the requirement to provide contraceptive medicines or services.
The Biden Administration will likely seek to have this ruling stayed until it is reviewed by an appellate court, and if this judge does not stay his order, seek a stay from the Fifth District Appeals Court or the US Supreme Court.
What this means for employers:
Most employers will not make mid-year changes in their plan designs; however, they may reconsider for 2024 and beyond if this ruling is upheld.
The costs of these preventive care services are relatively low, and the preventive care benefit is used by a large portion of the population. The preventive care requirement is a good example of “Value Based Insurance Design (VBID), where members pay less for high value services. It’s likely that uptake of preventive services would decrease if they were no longer covered without cost sharing.
An employer can continue to cover these preventive services at no cost share while awaiting a final ruling
I’ll cover the preventive care services that could be affected by this ruling in a future note.
1. Asthma inhalers cost a fortune even when they are off patent. Here’s why.
When I started in primary care practice in 1987, an inhaler for respiratory disease, asthma or obstructive lung disease, cost about $25 (which would be about $66 in 2023 dollars.) So, it’s a puzzle that inhalers for lung disease, which often have medication ingredients that have been off patent for years, often retail for $300-$400 or more. High prices for these inhalers make those with chronic persistent lung disease less likely to be adherent to therapy, which can lead to preventable hospitalizations and/or missed school or work.
Researchers in Health Affairs reviewed the 53 new lung inhalers approved since 1986, and found that pharmaceutical companies set up a “patent thicket” where there were an average of ten patents for each medication. Half (49%) of the patents were for the delivery device rather than the medication. In many instances extra patents were registered after generic companies had already filed for regulatory approval. Brand name pharmaceutical companies often sued generic manufacturers, and on average it took 13.5 years for the Food and Drug Administration to approve generics. The same research group reported earlier in JAMA that brand name pharmaceutical companies earned over $111 billion after the primary medication patent had expired on these inhaler drugs from 2000-2021.
Implications for employers:
Pharmaceutical companies increasingly are offering medications that are paired with a delivery system, which allows more patents to delay or avoid generic competition.
Reform of the patent system could lead to substantially lower costs for inhaler medications.
For High Deductible Health Plans, preventive drug lists may include certain inhalers which allow these medications to bypass the deductible, reducing financial access barriers
Employers can share links like this one to help them find affordable alternatives until there are legislative changes to make these costs more reasonable.
2. New frontiers in patient empowerment
There are over 14,000 cases of cervical cancer in the US each year. Researchers at Kaiser Permanente published a review of the economic implications of home human papillomavirus (HPV) test kits, a screening test for cervical cancer that can replace traditional pap smears. These researchers published clinical results of this large randomized clinical trial previously.
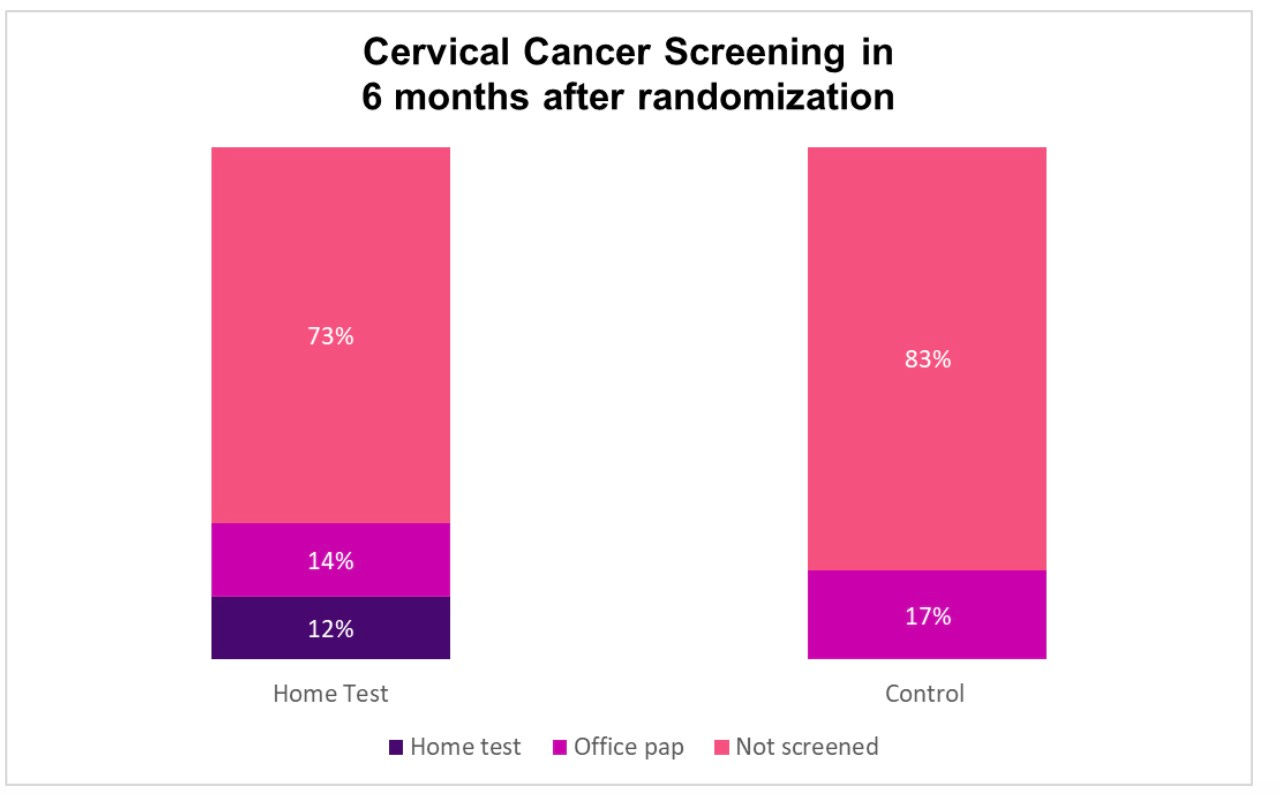
The clinical results are impressive. Researchers randomized almost 20,000 women from ages 30-64 who were not up-to-date on pap smears. They excluded women who had previous hysterectomies and therefore don’t need pap smears.
Only about one in eight who got the mail-in cervical swab returned it, but the portion of women screened was over 50% higher in the group that got this mailing. Over 50% more women who got the mailers had biopsies of suspicious areas of the cervix and abnormal findings, although this did not reach statistical significance. This home test is not as good as an in-person visit, where women can also be screened for sexually transmitted infections or domestic violence.
Source: Winer, et al JAMA Network Open 2019 LINK
The study published this week shows the economic impact of this study. The cost per additional screening was modest: between $86 (using internal Kaiser Permanente costs and $146 (using Medicare fee schedule).
Employer implications
The Food and Drug Administration has still not approved the home HPV swab as a cervical cancer screening test; when it is approved, employers can consider reimbursing for this test.
Employers could also offer these tests to members during January, which Cervical Cancer Awareness Month
As I mentioned in a note earlier this month, employers can deploy home colon cancer screening tests now.
It’s hard to engage members who have missed cancer screenings! While only 1 in 8 who got the home HPV test returned it, cancer screening tests still increased by 10 percentage points.
3. Patients appreciate rapid electronic access to their laboratory test results
Recent federal regulations require many providers to offer their patients electronic access to their medical records and laboratory results through a patient portal. A study in JAMA Network Open earlier this month shows that patients deeply appreciate access to their laboratory results. Researchers surveyed over 8000 patients at four academic medical centers who had viewed lab results in the previous month. Most (87%) saw lab reports before their clinicians informed them of results, and far more (46%) said that viewing lab results before their clinician made them less worried while few (7.5%) said it made them feel more worried. Ninety percent said they preferred lab result delivery through this patient portal, and 97% said they preferred seeing results as soon as they were available, even if their health care practitioner had not yet reviewed the results. One limitation of this survey is that Black people and Hispanic people were underrepresented.
Physicians sometimes worry that patient access to laboratory and medical records could cause unnecessary anxiety. This study suggests that patients want this access and I’m convinced that this can improve patient engagement, prevent missed abnormalities, and improve the quality of care.
Implications for employers:
Patients like access to their health information.
Home HPV tests and direct access to laboratory tests help make it “easy” for members to get the care and the information they need. This type of choice architecture is critical as we design interventions and benefit programs for members of employer sponsored health plans.
4. Blacks and low-income whites would benefit most from improvements in air pollution
Air pollution has significant adverse effects on human health. More air pollution causes not just asthma and lung disease, but also increases the chance of heart attack and premature birth, and decreases cognitive ability.
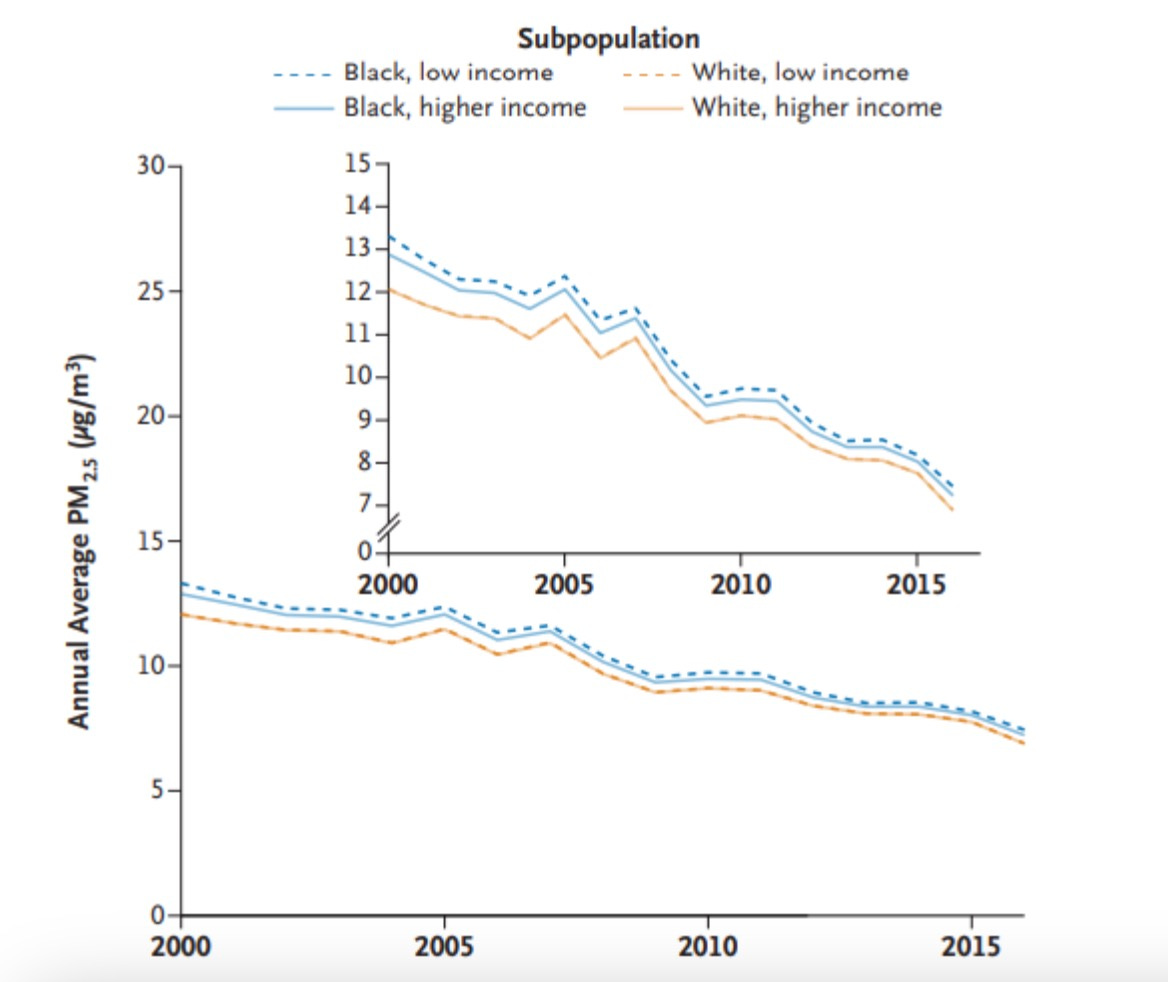
The New England Journal published research last Friday demonstrating that improvements in air pollution would help improve health equity by offering greater health benefits to Black people of all incomes and to White people with lower incomes - the groups that historically are most impacted by air pollution. The researchers analyzed 623 million person-years of Medicare data from 73 million enrollees over 65 - and correlated mortality to zip code level air pollution as reported by the Environmental Protection Agency.
The first piece of good news is that from 2000 to 2015, air pollution levels decreased overall (larger graphic) for every subgroup (top right inset). PM 2.5 refers to particles that are <=2.5 nanometers, which pose the highest risk.
Air Pollution Exposure by Race and Income
Source: Josey, et al New England Journal of Medicine March 24, 2023 LINK
No surprise that the researchers found exposure of Blacks and those who are poor had the highest exposure to air pollution, and seemed to benefit most from reductions in air pollution.
Implications for employers:
Decarbonization of our energy system in the US to combat climate change should further decrease air pollution, as we decrease use of fossil fuels in electricity generation, transportation, heating and cooling.
We should expect to see continued health and economic benefits from decreasing air pollution. Improved health equity could be an unexpected additional benefit.
Hope you have a great weekend when it comes!
Jeff