New treatments and challenges in obesity, Kaiser Family Foundation annual employer survey, and advances in infectious disease
November 4, 2022
Happy Friday.
Today, I’ll discuss new guidelines for obesity treatment in the context of expensive, newly-available drug treatment, implications from 2022 Kaiser Family Foundation annual employer survey, and some promising advances in infectious disease.
1. Specialty societies suggest expanding eligibility for drug and surgical treatment of obesity, and newly-available anti-obesity drugs are safe, effective, and pricey.
The prevalence of obesity is growing in the US and globally, and we increasingly understand that obesity is not simply a matter of “bad habits,” but is rather a metabolic disease that has many serious adverse outcomes, and often requires intensive medical intervention to address. We also know that most of those with severe obesity cannot sustainably achieve target weights through diet and exercise alone.
In the US (2018), 33.2% of adults have BMI of 30-35 (obesity) and 9.2% have BMI of over 35 (severe obesity). An additional 30.7% of the adult population is overweight - leaving only a bit over a quarter of the population at normal weight, BMI of 18-25.
For those with severe obesity, bariatric surgery helps lead to sustainable weight loss, and can reverse diabetes and dramatically decrease the risk of obesity-associated complications. Bariatric surgery has generally been limited to those with BMI>40, or those with BMI>35 and diabetes. At this point, most employers cover bariatric surgery, although they often require previous unsuccessful weight loss attempts. Bariatric surgery is best performed at a hospital with a multidisciplinary team, and many employers restrict this surgery to centers of excellence.
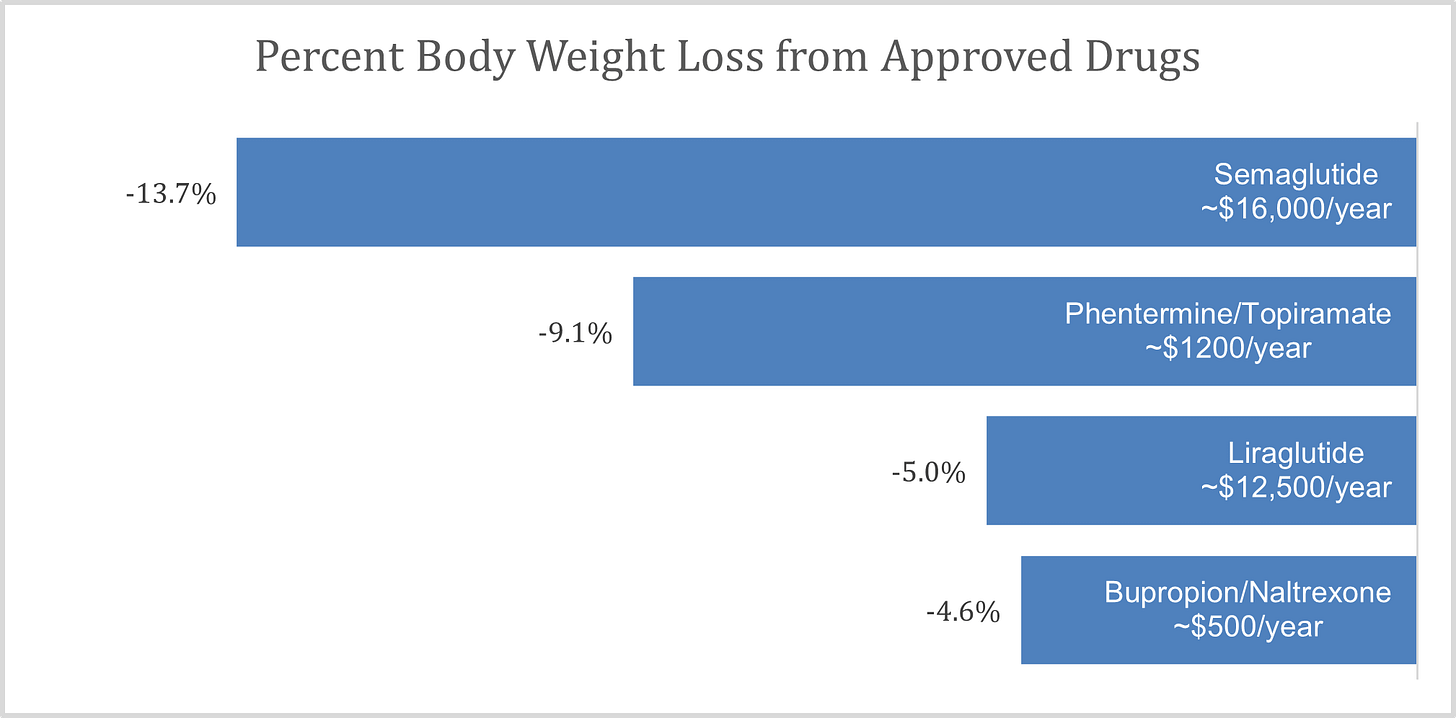
Until recently, medical therapy for obesity has been far less successful than surgery. Many of the available drugs have undesirable side effects and result in modest weight loss. Most diets do not lead to sustained weight loss of 10% or more of body weight, although ketogenic (ultra-low carbohydrate) diets such as the diet recommended by the vendor Virta Health have been successful for those able to maintain this type of restricted diet.
A relatively new class of drugs, initially marketed for diabetes, is associated with weight loss that rivals bariatric surgery, although this weight is regained if the drugs are stopped. The drugs can cause serious side effects, though these are rare. However, the drugs are very expensive! Their average wholesale price is about $15,000, and even after rebates they cost about $8000-$9000. Drugs in this class include liraglutide (approved in 2010 as Victoza for diabetes and in 2015 as Saxenda for weight loss), and semaglutide (Ozempic and Rybelsus for diabetes, and Wegovy for weight loss).
Another drug, tirzepatide (Mounjaro) was approved earlier this year and is on the market for type-2 diabetes and is likely expected to be approved for obesity by April 2023. These drugs are given as once daily or weekly self-injections. Rybelsus is an oral version of semaglutide given once daily, but only approved at this time for diabetes. The Food and Drug Administration (FDA) approved the weight loss drugs to be used as an adjunct to diet and exercise. Each of these medications is among the top cost drugs for our clients.
Sources: ICER.org, October 20, 2022 page 21 LINK. Prices from www.goodrx.com. Phentermine/topiramate and bupropion/naltrexone are available generically as separate pills.
Employers currently cover this class of medications for diabetes, and the majority of employers also cover doses marketed for obesity. But there are already press reports of widespread use of the diabetes drugs for weight loss among those who don’t have diabetes. If these drugs are used by a substantial portion of those with obesity, the increase in medical costs will be high. is currently in short supply, which could be contributing to the off-label use of Ozempic and Mounjaro. The shortage is expected to be resolved by the end of the year.
The American Gastroenterology Association, the professional society for gastroenterologists, recommended coverage of weight loss drugs for those with BMI >30, or BMI >27 with complications early this month. This recommendation mirrors the FDA approved labeling of these drugs and will increase pressure on health plan sponsors to cover these medications.
In this context, the two societies for surgeons who perform bariatric surgery, the American Society for Metabolic and Bariatric Surgery, and the International Federation for the Surgery of Obesity and Metabolic Disorders, just released new guidelines for bariatric surgery. Guidelines from 1991 recommended bariatric surgery for those with BMI >40, or BMI>35 with comorbidities like diabetes. Based on more recent data on long-term safety and effectiveness of surgery, they now recommend coverage of bariatric surgery for those with BMI>35, or >30 with related problems like diabetes.
These societies also recommended coverage of bariatric surgery for children or adolescents who are more than 140% of the 95th percentile, or 120% of the 95th percentile if they have diabetes or other complications. Long term follow-up of children or adolescents who have bariatric surgery demonstrates sustained weight loss without negative impact on bones or sexual development.
Implications for employers
- The tools to address severe obesity are much improved, but the cost of this treatment is likely to be large.
- These advances are coming at an excellent time for patients, who need them more, but at a difficult time for employers already facing the highest medical inflation rate in decades.
- Bariatric surgery is a higher initial expense, and there is a track record of safety for decades.
- This new class of medications cost less than bariatric surgery in the first year, but the cost over less than three years would generally be higher than the cost of bariatric surgery. Long term experience with this class of drugs is very limited.
- Ketogenic diet might be a good alternative to bariatric surgery or these new medicines for those able to maintain this diet.
- If adding drug coverage, consider sponsoring lifestyle modification benefits (such as diet and exercise) in line with the FDA approved intended use of pharmacotherapy.
- Consider making bariatric surgery available to children or adolescents, as appropriate.
2. KFF survey shows little change in health insurance design and costs in 2022
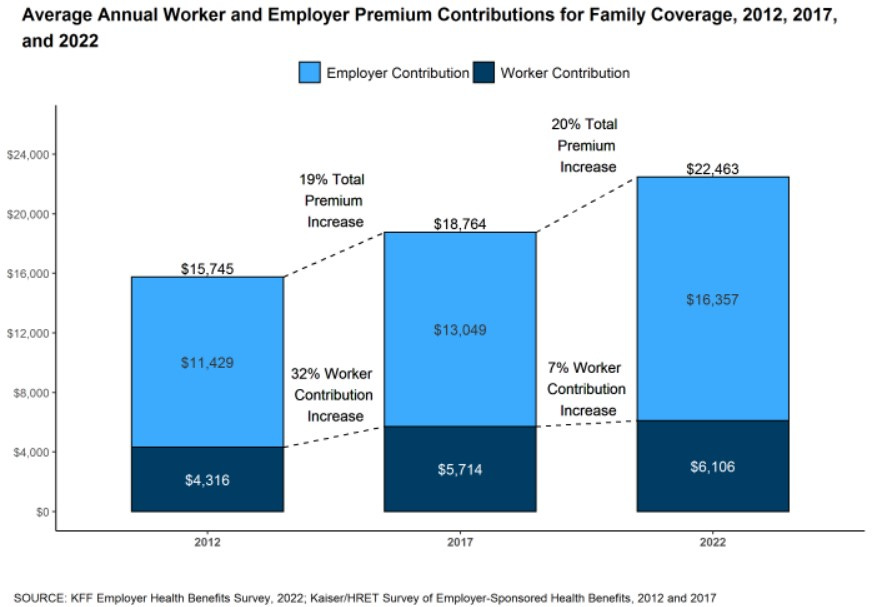
KFF, previously called the Kaiser Family Foundation, released its annual survey of over 2000 employers reporting on their 2022 health plan cost and design. Premiums are about $8K (single) and $23K (family) and are not much changed from 2021. Premiums are up 20% over the last five years. Cost sharing is not much changed from 2021. This is the first 5 year period in the history of this survey where worker earnings went up more than premiums.
Source: KFF October 30, 2022 LINK
The KFF researchers also found that penetration of high deductible health plans (28%) is not much changed in the last five years, and prevalence of narrow networks (29%) is modest. They found affordability remains an issue. A quarter of workers at small firms (<200 employees) pay more than $12k in premiums, and average deductibles were $1763 (single) and $3000-$4800 (family).
Implications for employers:
- While plan design and cost were mostly unchanged in 2022, the current high rate of medical inflation will likely mean much larger changes in 2023.
- A combination of long-term consequences of missed care during the pandemic, provider consolidation, and multi-year provider system contracts that delay the impact of inflation means that high medical inflation will likely persist in 2024 and 2025.
- Employers should plan now for efforts over the coming few years to address medical inflation in the context of a tight labor market.
3. Assorted good news on the infectious disease front
A) Respiratory Syncytial Virus (RSV) has overwhelmed pediatric hospitals in many communities this fall. Pfizer announced that results of a trial of a new RSV vaccine given to women in pregnancy to protect their newborns born during RSV season. The vaccine prevented 82% of hospitalizations in children under 3 months old, and 69% of hospitalizations in children under 6 months old. Pfizer has also published data showing effectiveness in older adults, who are most likely to die of RSV. An RSV vaccine would be great news to prevent serious illness and death among both infants and the elderly.
B) Malaria kills over 600,000 a year, mostly children, and mostly in Africa. Mosquito control and netting can prevent disease in many, but daily or weekly preventive medicines are hard to administer to large populations in developing countries. Researchers report that a new monoclonal antibody is 88% effective at preventing malaria for six months in healthy adults. Research subjects were tested for malaria every two weeks; 78%in the placebo group had malaria during the 6 month malaria season compared to 18% of those who got the infusion. Administering 30 minute intravenous infusions broadly in developing countries is not feasible, but this or a similar medication administered through a simple injection could dramatically improve health in sub-Saharan Africa.
C) A positive note about potential future COVID-19 vaccinations. Researchers at Yale showed that an intranasal vaccine induced substantial immunity in the upper airway, which could be far more effective at preventing transmission of COVID-19. China and India have each approved inhaled or nasal vaccines, although these could still be years away in the US, and ‘real world’ effectiveness data has not yet been published.
D) A Boston company just raised $27 million to continue its research on a skin patch with microneedles made of silk proteins to deliver influenza vaccines. This is not nearly ready for market, but this promising technology could make getting vaccinations much easier, even for those without needle phobia.
Have a great weekend.
Jeff