Peterson Institute releases its report on virtual programs for depression and anxiety
June 23, 2025
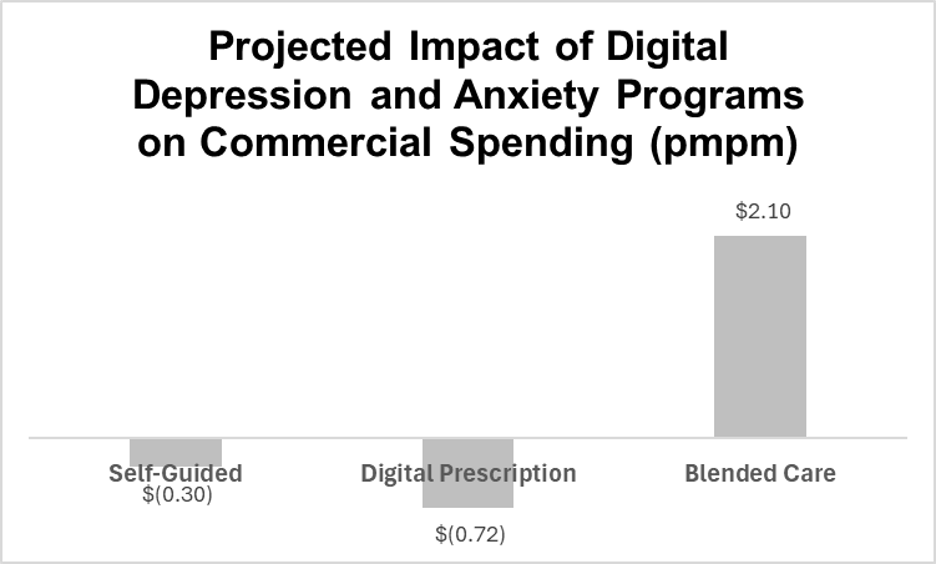
Summary: Researchers found that digital health solutions improve clinical symptoms of depression and anxiety. Self-guided solutions and prescription therapeutics could lower total medical claims costs, but solutions that include access to live coaches and therapists likely increase medical claims costs.
Source: Peterson Health Technology Institute, June, 2025
The Peterson Health Technology Institute released its report on digital mental health services earlier this month. The Peterson Institute, funded by a large grant, has previously published reviews of the efficacy of musculoskeletal solutions, diabetes solutions, and hypertension solutions. The Institute reviews peer-reviewed and “gray” literature (published by companies or think tanks), as well as materials provided by each of the vendors evaluated.
The Institute reviewed the efficacy of three types of mental health interventions: self-guided programs (an app used by health plan members), digital prescriptions (an app approved by the FDA which requires a physician prescription), and blended care (an app or digital program combined with access to human coaches and therapists).
The Institute also provided research data that shows that patients with more severe anxiety or depression have higher medical costs. See these charts:
Source: Peterson Health Technology Institute, June, 2025. Data from Culpepper, et al 2024
Source: Peterson Health Technology Institute, June, 2025. Data from Kavelaars, et al 2023
Then, the Institute built a model which assumes that a decrease in symptoms of depression or anxiety, using well-validated PHQ-9 and GAD-4 surveys, would be associated with lower medical claims costs. That’s not a certainty, since those who have better-treated severe depression might still have higher medical claims costs than those who had only mild depression in the first place. There are similar challenges with some models that would predict lower costs of those with diabetes in those who were treated and achieved a lower HbA1C level. The correlation of lower cost to lower HbA1C does not prove causality.
They used their economic model to project the likely impact of the three types of interventions on medical claims costs of an employer-sponsored health plan. They projected that due to low estimated program costs, self-guided and prescribed digital therapeutics would lead to,lower total expenses, while hybrid programs that included human coaches and therapists would increase plan expenses.
Implications for employers:
Plan members with severe anxiety and/or depression have higher total medical claims costs than those with mild or absent symptoms.
The Peterson Institute found that digital programs to treat depression and anxiety were clinically effective. This is especially important given shortages of mental health clinicians.
Cost-effectiveness of programs was highly dependent on program costs and engagement rates. Programs could be cost saving if they were either less expensive or if they engaged a larger portion of the population.
Employers should carefully review performance guarantees that include a promise of return on investment (ROI) to be sure that they agree with the vendor’s methodology of calculating ROI.
Programs that clinically improve anxiety and/or depression could improve work productivity and provide substantial value even if they don’t decrease medical claims costs. Effective digital solutions can improve access to scarce mental health resources.