Price still driving increased health care costs, out-of-pocket costs for pediatric hospitalizations, and physicians and patients assess virtual care.
April 28, 2023
Today, I’ll review findings from the Health Care Cost Institute’s 2021 health care cost and utilization report, which shows that unit cost increases represented two thirds of the total cost increase from 2017 to 2021. I’ll also examine the out-of-pocket costs of pediatric hospitalizations, and discuss data from a just-published survey of physicians and patients to gauge their desire for virtual care.
But first, be sure to check out my article in Harvard Business Review this week on what employers can do to improve the safety of childbirth in the US.
1. HCCI shows that price increases represent about two thirds of health care spending increases from 2017-2021
The Health Care Cost Institute (HCCI) recently published data on health care spending, utilization, and average prices from 2017 through 2021 for individuals under the age of 65 who receive health insurance coverage through an employer. HCCI analyzes deidentified claims data from about 55 million members (Aetna, Humana, and BCBS plans) to assess what is driving health care cost spending. Their analysis has shown that unit price increases have driven the rise in total expenses, although in 2021 utilization increases were high, largely due to depressed utilization in 2020 due to the pandemic.
In this chart, you can see that unit prices have increased by about 14% from 2017-2021, while utilization increased only 7%. This is why health care economists rally around the statement that “It’s the Prices Stupid” when asked why medical care in the US is so much more expensive than in other developed countries.
Source: HCCI, April, 2023 LINK
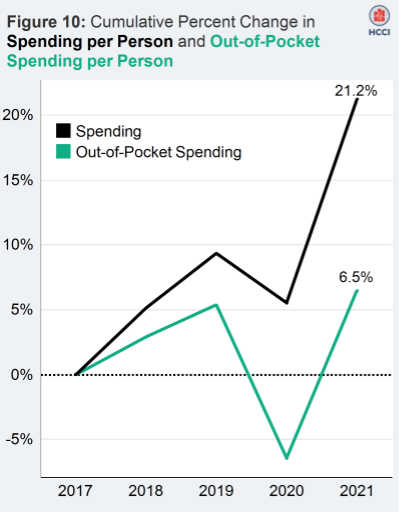
While members facing high out of pocket costs sometimes complain that the value has been stripped out of their health plans, the HCCI data shows that cost increases borne by employers have been three times larger (21%) than cost increases borne by employees (7%).
Source: HCCI, April, 2023 LINK
The chart below deconstructs the reasons why costs have increased by categories of service. For instance, on the left you see that hospital costs (red) are up 20% from 2017-2021. The components of this increase on the right are a decrease in hospital days of 6% but an increase in cost per day of 28%. This is data from 2021, so it doesn’t include recent increases in hospital contracted fees based on increased hospital staffing and supply costs.
Source: HCCI, April, 2023 LINK
HCCI does not have information on rebates, so cost increases in pharmacy are somewhat overstated as rebates made up a larger portion of total costs in 2021 compared to 2017.
Implications for employers:
- The increase in medical costs in the US is largely due to increased unit costs, rather than increased utilization.
- This data shows the importance of programs that reduce unit cost, such as programs to encourage use of high value providers, bundled pricing and moving services away from hospitals to free-standing centers.
- Employers should seek carriers which achieve net lower prices from providers.
2. Families face high costs when their children are hospitalized
Luckily, most children are healthy and each year relatively few children are hospitalized. But recent data shows that when kids are sick enough to be hospitalized, their families incur substantial out-of-pocket costs.
Researchers in JAMA Pediatrics reviewed claims from almost 10 million children with almost 200,000 hospitalizations from 2017-2019, and found that on average out-of-pocket cost for pediatric hospitalizations was $1313, and out-of-pocket cost exceeded $3000 for more than one in seven kids hospitalized. The researchers matched patients where possible to what type of health plan they had and found that those with high deductible health plans faced the highest out-of-pocket costs. This doesn’t fully account for the financial damage to families whose children are hospitalized. Parents often lose income when they miss work, and the costs of medicine, outpatient care, and even parking, further stress family finances.
Source: Carlton, et al JAMA Pediatrics March 27, 2023 LINK
Implications for employers:
- Careful health plan design considering resources of members can help prevent financial insecurity due to hospitalizations.
3. Patients and primary care physicians ambivalent about virtual care
Health Affairs just published results of a set of surveys performed in mid-2021 asking both patients (1417) and primary care physicians (337) how they felt about video and audio visits. More patients (33%) and many more physicians (61%) felt that the quality of virtual visits was lower than in-person visits, and a majority of each preferred that all or most future visits were in person. Still, almost twice as many patients (36%) preferred that future visits be virtual compared to physicians (19%).
Source: Steelfisher, et al Health Affairs April, 2023 LINK
Source: Steelfisher, et al Health Affairs April, 2023 LINK
Some might cite this study as evidence that ambulatory visits will return to the office as they were pre-pandemic, but I’m not so sure. The study was conducted almost two years ago, and providers got better at doing virtual care since Spring, 2021. Further, the researchers did not differentiate video from audio-only visits, so we don’t know if perception of quality or rapport was different with video. Most virtual visits are now for mental health; this study sought opinions of only primary care physicians.
Implications for employers:
- Patients can benefit from virtual care, which eliminates travel time, parking costs, and offers access to more diverse providers.
- I believe virtual care is here to stay, and that if ‘brick and mortar’ providers aren’t willing or able to deliver this, more care will be delivered by providers that are not part of the traditional medical system.
Hope all have a good weekend when it comes.








Jeff - what impact has the reduced reimbursement rates from CMS and Medicaid programs have in the price increase from hospitals? Also if employer sponsored plans are making every effort to reduce inpatient stays doesn’t it reason the hospital per unit costs would need to increase since the number of units has deceased