Primary care shortage likely to continue
November 25, 2024
Summary: Much-needed primary care clinician growth will most likely come from advance practice clinicians (physician assistants and nurse practitioners, and employers should be prepared for continued access challenges.
Source: Bazelman J Gen Int Med, October 23, 2024
I’m a primary care physician by training, and I loved practicing primary care. Primary care physicians can help patients navigate our confusing health care system, keep up with preventive care, and make difficult health care decisions that are consistent with their wishes and values. As a patient, especially as I get older, I value my visits with my primary care physician.
But I’m lucky. Many people cannot find a primary care physician. Wait times to get an appointment for a new pediatrician, general internal medicine physician, or family physician are often over a month, and many primary care clinicians are not seeing new patients.
And things are getting worse. Physicians in training are not choosing to go into primary care; a record number of training positions in primary care fields went unfilled in this year's residency match. The pipeline for training new PCPs is long; residency is at least three years, and most medical students have decided whether to pursue primary care by the middle of their third year of medical school.
There is one bright spot. Nurse practitioners (NPs) and physician assistants or physician associates (PAs) represent most of the increase in primary care capacity over the last decade. But even NPs and PAs are increasingly considering joining specialty practices instead of going into primary care. While traditional NP programs required years of clinical practice, Bloomberg Businessweek reported that some graduates of newly accredited remote nurse practitioner training programs receive little clinical training during their education, and some of these programs require no previous clinical experience.
Source: Bazelman J Gen Int Med, October 23, 2024. This shows that total visits provided by physicians decreased slightly during this time period.
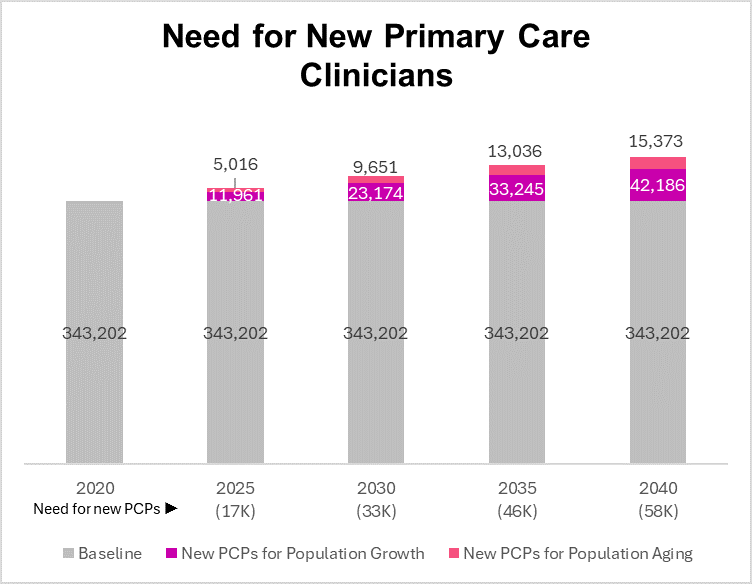
A report in the Journal of General Internal Medicine used data from the Medical Expenditures Panel Survey and databases of physicians, NPs and PAs to estimate current primary care clinician counts, and project how many net new primary care clinicians are needed by 2040. They found that about 58,000 new primary care clinicians are needed to meet the population needs by 2040.
We are unlikely to train this many new primary care physicians by 2040, so many of these services will need to be provided by non-physicians. Some hoped that new tuition-free medical schools could encourage more physicians to pursue primary care training but preliminary data shows that graduates of these programs go into primary care less often than graduates of programs that charge tuition. Another potential solution is foreign-trained physicians who could help meet this need. Some states have made it easier for foreign-trained physicians to practice, although immigration restrictions could decrease the supply of foreign medical graduates.
Implications for employers:
It’s likely that primary care services will increasingly be provided by PAs and NPs, with physicians playing a smaller role.
Health plan designs that require primary care physicians might have difficulty obtaining adequate coverage.
Virtual care can help primary care clinicians support a larger patient panel, which could alleviate the potential shortage.
Employers should encourage carriers to limit prior authorization and other hassles for primary care clinicians.
Thanks for reading. You can find previous posts in the Employer Coverage archive
Please subscribe, “like” and suggest this newsletter to friends and colleagues. Thanks!
Tomorrow: Tirzepatide may improve outcomes in adults with congestive heart failure (by my colleague Patricia Toro, MD MPH)