Provider directory inaccuracies persist
June 18, 2024
Directory inaccuracies in follow up “secret shopper” survey
Source: Haeder, SF Health Affairs Scholar, June, 2024 LINK
Health plan members use health plan electronic directories to determine which health plan to enroll in, and whether a provider is in-network has huge implications for member out-of-pocket responsibility. A mistake in a provider directory can mean a patient will lose access to their provider or could incur thousands of dollars in out-of-pocket costs. Consumer advocates have complained about inaccurate provider directories for years, and the No Surprises Act requires health plans to update their provider directories at least every 90 days.
Health Affairs Scholar published research this month showing that even when health plans are informed of directory errors, it takes a long time for them to be corrected.
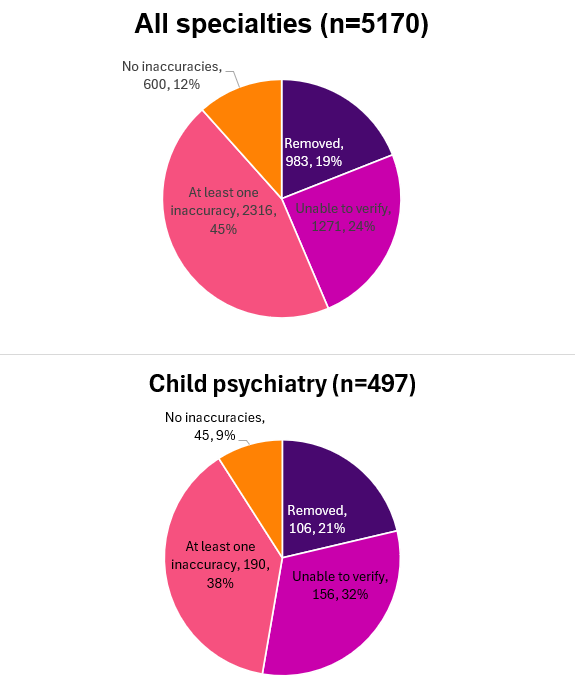
Researchers performed secret shopper calls in spring, 2023, and identified 5,453 providers in eight Pennsylvania Affordable Care Act marketplaces whose provider directory entries were erroneous. The errors included listing an out-of-network provider as in-plan and incorrect address, phone number and specialty. They resurveyed 5,107 of these providers in December 2023 and early January 2024 (between 117 and 280 days after the initial survey) and found that only one in eight providers (12%) now had no inaccuracies in their directory entries. The problem was similar in child psychiatry, although the researchers were unable to verify health plan directory accuracy on a larger portion of the providers.
There were substantial differences among the carriers. One plan achieved 35% of providers with no directory error, while another achieved under 9% with no directory error. The researchers found that 3.7% of providers listed in directories were actually out of network; this ranged from 1.7% to 6.7% among the eight carriers. These findings might not be applicable to all carriers; the analysis was restricted to ACA plans in a single state.
Implications for employers:
Provider directories are an important function of health plans, and employers can continue to press their carriers to regularly verify and correct their provider directories.
Members rely on provider directories to help them choose health plans and providers, and employers will likely face disgruntled employees or pushback if members have acted on incorrect directory information.
Directories work best if they can accurately statewhether a provider is taking new patients. Employers can ask carriers if this is noted accurately in the directory.
Thanks for reading. You can find previous posts in the Employer Coverage archive
Please subscribe, “like” and suggest this newsletter to friends and colleagues. Thanks!
Tomorrow: FDA committee gives thumbs down to MDMA for PTSD