Resident “Match Day,” pharmaceutical price drops, prior authorization, and COVID-19 risk continues to decline.
March 24, 2023
Happy Friday!
Today, I’ll talk about some surprises about 2023 enrollment in training programs for new physicians, what’s behind the recent drops in insulin prices, growing physician and policymaker anger about prior authorization, and good news (mostly) about COVID-19.
1. Annual “Match Day” shows that emergency and family medicine programs look unattractive to new physicians
The third Friday of March is “National Resident Match Day,” where every graduating medical student finds out where they will spend the next three or more years of training. Fourth-year medical students apply to and interview at residency positions in different specialties all over the country, and they rank and are ranked by training programs. A computer program goes through many thousands of iterations to find the statistically best match for each medical student.
It’s a grueling and stressful time for young physicians-to-be. There were about 15% more applicants than there were positions this year; those who do not match can “scramble” to find an empty position in another program, or do research or other work for a year and then apply the following year.
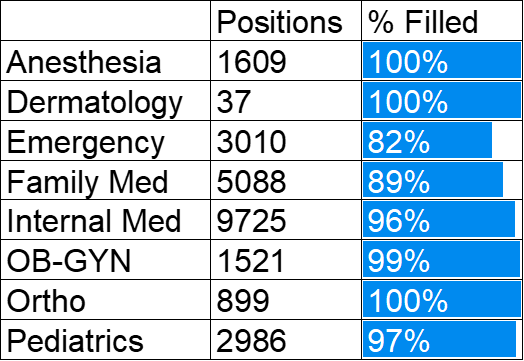
Primary care has had a hard time in “the match” in recent years, with general internal medicine and family medicine programs failing to completely fill. Almost half of the family medicine positions were filled by those who received their medical training outside of the US. Training programs in radiology and dermatology and plastic surgery tend to fill easily. These specialties are highly paid and often have flexible schedules. Here’s a look at the results of this year’s match:
Source: National Residency Match Program LINK
The big surprise this year is that 46% of emergency medicine programs failed to fill, and 18% of positions were empty at the conclusion of the match. This is dramatically worse than previous years (see below). There are likely many factors driving low rate of matching in emergency medicine. This includes an increasing number of programs and worries that private equity companies will decrease hiring and pay. Three years of pandemic and jam-packed hospitals with patients “boarding” in emergency departments for days waiting for inpatient rooms have also taken a toll on emergency medicine physicians.
Source: Bryan Carmody via Twitter
Implications for employers:
- The scarcity of emergency medicine trainees increases the importance of efforts to avoid preventable emergency department visits. Fewer emergency medicine physicians could also increase future emergency department costs.
- The shortage of new physicians entering family medicine bodes poorly for efforts to center health care reform around deep continuity relationships with attentive primary care physicians. It’s likely that more primary care will be delivered by advanced practice clinicians (nurse practitioners and physicians assistants).
- The shortage of primary care physicians will be a special problem in rural areas. It’s likely that many of the unfilled residency slots were in smaller more rural hospitals, and physicians are most likely to practice in underserved areas if they grew up there or if they train there.
2. Recent drops in insulin prices show that federal policy and competition can impact the commercial market
Eli Lilly, Novo Nordisk and Sanofi manufacture almost all of the insulin sold in the United States, and so far this month each has announced price cuts of around 75% on some of the older insulin products that they sell. Lilly and Sanofi have also announced programs to cap out-of-pocket payments by people with diabetes who have commercial health insurance, too.
This is unabashed good news, although many people with diabetes who have commercial health insurance won’t see much difference. That’s because many employers already have programs that cap out-of-pocket costs - so they already pay no more than $35 monthly for insulin. Employers will be relieved to have this out-of-pocket limit covered by the pharmaceutical company.
What led to these price cuts?
Increasing public pressure on the pharmaceutical companies certainly helped, and stories in the press about young adults with Type 1 diabetes dying after they rationed their insulin are horrifying. The manufacturers also faced competitive pressure from Civica, a nonprofit owned by hospital systems which just was hired to manufacture generic insulin by the state of California.
There is one more pressure that is easy to overlook. Pharmaceutical companies are required to offer state Medicaid programs rebates if they do not receive the lowest price in the market or if their prices rise more rapidly than inflation. Until now, those rebates were capped, but new rules that take effect on January 1, 2024, would mean that pharmaceutical companies could have owed Medicaid programs so much that they would have had to pay the government for each vial distributed. So the major manufacturers of insulin decided they preferred steep price decreases to owing large rebates.
Implications for employers:
- Federal policy can help make pharmaceutical agents more affordable, even if the federal government right now is not allowed to set prices or negotiate for drug products for the commercial market.
- Future Medicare negotiations over the most expensive outpatient drugs and Medicare rebates for drugs with excessive price increases could also help lower commercial costs, although we’ll have to watch launch prices carefully.
- While these price cuts for insulin are a relief, large increases in pharmacy spending are likely in the coming years due to improved genomic therapy and new effective drugs for diseases including obesity.
- Employers can track their formularies to be sure that their members and their plans benefit from these price cuts.
- Lower list prices for insulins could potentially reduce rebates, although this is still to be determined. Financial models will need to account for these changes in the years ahead.
3. Physician survey increases pressure on prior authorization programs
The American Medical Association has been getting a lot of play from a survey of physicians, who said unsurprisingly that they hate prior authorization requirements. This is no surprise - prior authorization programs create extra work for physician offices, and some of the programs are especially frustrating, as physicians in different fields are reviewers, or as insurance companies simply deny based on an algorithm, rather than based on the actual patients’ circumstances. Further, some Medicare Advantage programs have apparently been disregarding Medicare rules when they issue denials. Provider burnout is a serious problem, and poorly designed or executed prior authorization programs can be one more obstacle to an overworked physician finishing their day.
Source: American Medical Association March, 2023 LINK
Well-designed prior authorization programs can help decrease variation in care and decrease medical waste. Prior authorization programs can even help protect members against potentially harmful therapy. Many employers feel they can only afford to offer coverage for some discretionary care if they implement prior authorization programs, and prior authorization for elective outpatient CT scans and MRIs is almost universal. Prior authorization can also help direct members to more cost-effective outpatient facilities, or to providers with better surgical outcomes.
Many states have limited prior authorization by statute or regulation, although this only affects fully insured plans regulated by the state. About two thirds of employees are in self-insured plans, which are not subject to state laws.
Here’s a link to a Kaiser Health News report on increasing policymaker interest in prior authorization.
Implications for employers:
- Employers can help ‘turn down the heat’ by overseeing their carrier and pharmacy benefit manager programs to be sure they don’t create unreasonable work or hardship for patients or ordering physicians. This includes limiting prior authorization to areas of high impact, where inappropriate care is common.
- Employers can make health plan members aware of appeals rights, and exclude emergency diagnostic and therapeutic interventions from prior authorization
4. COVID-19 risk of hospitalization and Long COVID appears to decline
This is the first week that influenza-like illness (which includes respiratory infections such as COVID-19) is below “baseline” level. As you can see below - we had a lot more illness early this season, and have gotten down to baseline levels of influenza-like illness earlier than usual.
Source: Centers for Disease Control and Prevention March 21, 2023 LINK
There are some other heartening reports
- Wastewater levels of the virus which causes COVID-19 continue to decline nationally.
- We have not seen the emergence of new variants that are either much more dangerous or much more transmissible. China’s decision to eliminate all pandemic restrictions did not unleash multiple new variants
- Infection with Omicron appears to be less dangerous than infection with the initial virus or earlier strains. Some of this might be due to an increasing amount of immunity from both vaccinations and infections.
- Estimates of new cases of Long COVID are coming down. This could be due to differences in prevalent strain, more immunity, or more use of Paxlovid, which reduces risk of Long COVID. It also appears that new disability claims from Long COVID are also declining.
- A randomized controlled trial showed that the antidiabetes drug metformin lowers the risk of Long COVID. If these trial results are confirmed, metformin could join vaccination and Paxlovid as effective ways to prevent Long COVID.
Implications for employers:
- The virus which causes COVID-19 is still circulating, and employees should still have access to tests and sick leave if they need it.
- Even with estimates of Long COVID rates going down, many employees and family members have cases of Long COVID. Companies will need to continue to offer reasonable accommodations to employees who continue to have symptoms.
Hope all have a great weekend when it comes!
Jeff