Should employers encourage more prostate cancer screening?
June 11, 2025
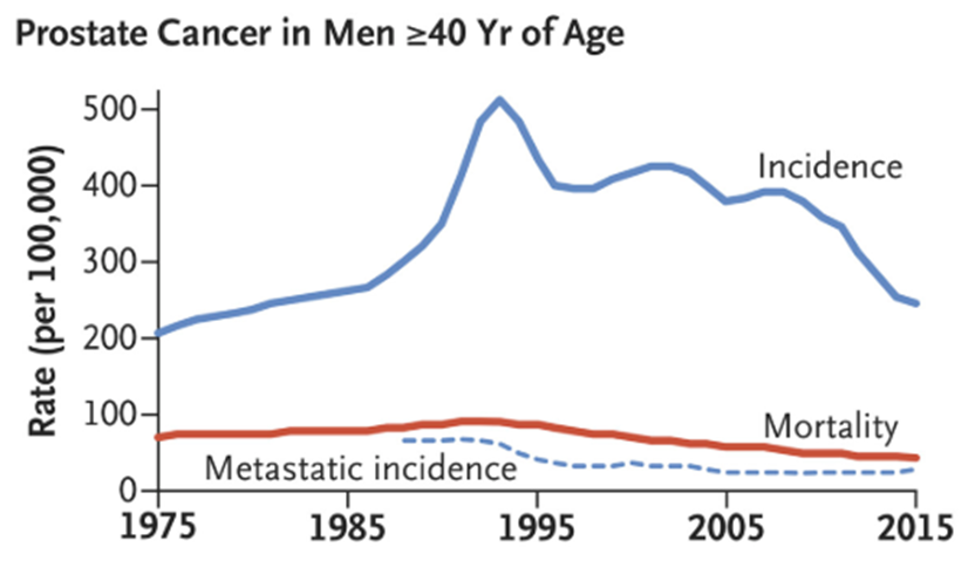
Source: Welch, et al NEJM 2019. Widespread PSA screening for prostate cancer began in 1986- just before the peak of incidence. Note that fewer cases of metastatic disease were found, and mortality from prostate cancer declined modestly.
The diagnosis of former president Joe Biden with aggressive prostate cancer last month raises the question for many men about whether they should be screened. Reporting may also make some employers wonder if they should institute programs to encourage prostate cancer screening.
Prostate cancer is common - and rates of prostate cancer rise dramatically as men age. Prostate cancer is the second leading cause of death from cancer in men; lung cancer remains the number one cause of cancer death in men. However, screening for cancer should only be recommended when the screening is associated with longer survival or improved quality. Cancer screening can cause harm, too. Treatment for prostate cancer with radical prostatectomies is associated with urinary incontinence and erectile dysfunction.
We intuitively believe that early detection for cancers will save lives, but some cancers grow so slowly that finding them doesn’t improve life expectancy. Also, some cancers grow so quickly that they can rarely be found before they have spread, and earlier detection might lead to longer treatment without longer life. Many prostate cancers unfortunately are in these categories where screening does not improve quality of life or life expectancy.
Two large studies of prostate cancer sceening over a decade ago yielded divergent results. A U.S. study showed no statistically significant survival advantage of screening, and a European study showed decreased risk of death from prostate cancer with screening but no overall change in survival. More recent studies point to a very modest survival advantage, although between 540 and 1100 men must be invited for screening for every life saved.
The U.S. Preventive Services Task Force recommends that men talk to their clinicians about whether they should be screened for prostate cancer from the ages of 55 to 69, and recommends against prostate cancer screening in those aged 70 and over. Men with a family history of prostate cancer should likely be screened, and Black men are more likely to die of prostate cancer and may consider screening. The American Urologic Association recommends prostate cancer screening every 2-4 years from ages 50 to 69.
Implications for employers:
Employers can continue to waive cost sharing for PSA testing for prostate cancer screening even though this is not recommended by the USPSTF.
Some employers have incentive programs for men to get prostate cancer screening; however, such an incentive program might undermine the shared decision-making between the member and his clinician.