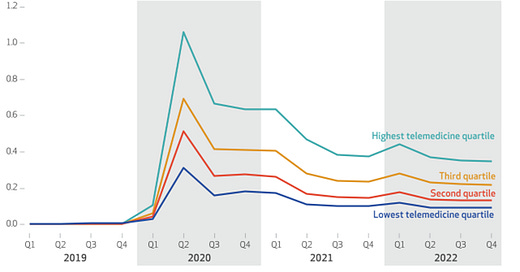
Telemedicine visits per quarter by quartile of provider telemedicine use
Source: Nakomoto, et al Health Affairs, May, 2024 LINK
Researchers compared costs and some elements of quality in Medicare beneficiaries in health care delivery systems that had the highest and lowest use of telemedicine during the pandemic and found that the providers with the highest amount of telemedicine services had slightly higher costs (1.6%). Providers that delivered more telemedicine had 2.7% fewer emergency department visits, which was statistically significant. Medicare beneficiaries cared for by the health systems with the largest amount of telemedicine had a 2.3% higher rate of hospitalizations. This did not reach statistical significance but drove a large portion of the increase in costs. More of the high telemedicine providers were academic medical centers or in the Northeast, so the researchers excluded COVID-19 visits and hospitalizations as these occurred at different rates and times in different geographies.
This research, published in Health Affairs, also noted an increase in adherence to metformin (a medicine for diabetes and prediabetes) and statins to lower cholesterol. There was no significant difference in rates of cancer screening. There were significantly fewer laboratory and imaging tests within seven days of a telemedicine visit, but overall lab and imaging test rates in the high and low quartile telemedicine systems were not significantly different.
This research used a large sample, 100% of those on traditional Medicare. Medicare beneficiaries have a different pattern of care than those on commercial insurance, including far more visits and hospitalizations. This research suggests that going to a provider with more telemedicine access does not dramatically increase visit volume or total cost, but in a high-risk population it is not likely cost saving. The authors note that the high telemedicine providers might have had limited capacity that helped tamp down utilization.
Implications for employers:
- This research suggests that maintaining current access to telemedicine will likely mean costs will be slightly higher, disappointing those who felt that telemedicine would result in sharply lower total costs.
- Telemedicine visits for mental health services represent a majority of telemedicine use in commercial plans in many geographies now, and this study did not focus on mental health services.
- Telemedicine is likely to play an increasing role in access to mental health as well as primary and some specialty care.
- Employers should think about telemedicine as a vital portion of the medical care delivery ecosystem and continue to monitor its utilization and impact on care.
Thanks for reading. You can find previous posts in the Employer Coverage archive
Please subscribe, “like” and suggest this newsletter to friends and colleagues. Thanks!
Tuesday: Proton beam therapy coverage considerations (By Patricia Toro, MD MPH)
In Memorium:
The world of health policy lost a giant with the untimely passing of Suzanne Delbanco. She was the founding executive director of the Leapfrog Group, convening employers together to seek greater accountability for accountability from providers. I had the honor of working with Suzanne as she founded Catalyze Payment Reform, which brings health purchasers together to demand improved payment methodology to both improve quality and control costs. Suzanne built an impressive team, and kept her eye firmly on the goal of demanding payment that would promote high value care. She obtained foundation sponsorship to support rigorous research, and she had a podcast before everyone had a podcast. She was especially passionate about improving maternal quality and safety, and her enthusiasm motivated me and so many others.
Here’s a link to the CPR tribute to Suzanne, and here’s a link to a tribute from our mutual friend Francois de Brantes. The world was a brighter place with Suzanne’s passion and her smile, and we will all miss her greatly.