Value based payment works best when it’s “high intensity”
June 20, 2023
Source: Pandey, A et al Health Affairs June, 2023
We all would prefer to “pay for value,” and health care policymakers advocate movement away from fee-for-service (FFS) payments. FFS payment is the dominant payment method in the US and around the world, but it can promote overutilization of lower value (but higher margin) care. However, there are relatively few studies that have examined the impact of value-based payment.
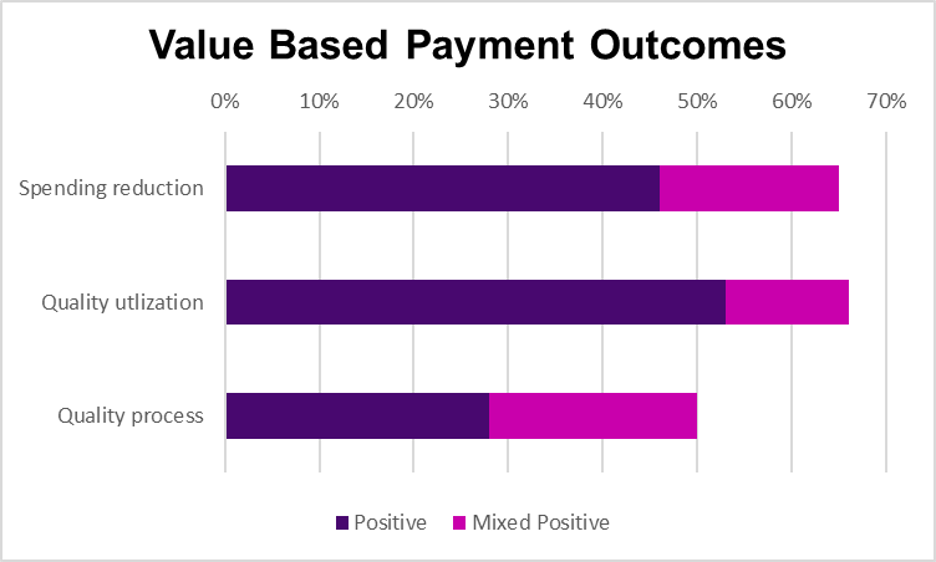
Health Affairs published a review this month of the 24 programs they found which provided incentives for lowering costs and raising quality through 2020. Of these, only a single study was a randomized controlled trial (the Medicare Comprehensive Joint Replacement Program). Nine programs were determined by the researchers to be high intensity (upside or downside risk, minimum quality standards to receive any payout). Ten were government programs (Medicare or Medicaid)
Many of the value-based payment programs included substantial nonfinancial support, including data analysis (22), technical assistance (20), infrastructure payments (12), raw data (15), risk management support (8) and care management (7).
The researchers found that the highest intensity programs were most likely to yield positive results. They note that there is likely publication bias - researchers are more likely to publish articles on programs that were at least in part successful.
Implications for employers:
- There is no guarantee that “pay for value” programs will either save money or improve quality.
- Health plans should likely provide substantial support for providers to help them succeed in pay for value programs, and employers should expect carriers to demonstrate that they are providing appropriate support for providers to succeed in “pay for value” programs.
- These programs are a heavy lift for carriers and for providers, and are most feasible where a health plan has a large market share. Employers should ask hard questions of plans that promise to implement pay for value programs in geographies where they have relatively few patients.
- Setting up a plan to monitor results is important; even well-designed programs often need to be adjusted once put in place to get the desired outcome.
Tomorrow: Many local pharmacies don’t stock medications to treat opioid use disorder