What the end of the pandemic emergency will mean for employers, Paxlovid and Long COVID, and two studies on sick leave
November 11, 2022
Happy Friday,
Today, I’ll discuss the implications for the end of the pandemic emergency for employers, impressive new data that Paxlovid decreases incidence of Long COVID, and two studies of implication of sick leave mandates.
1. Implications of the end of the Pandemic Emergency for employers
The COVID-19 pandemic emergency was declared on January 31, 2020, and it has been extended regularly since. The end of the emergency is expected sometime in 2023, and the Biden Administration has promised to provide 60 day notice. The emergency is currently set to end on January 11, so we will find out later today (November 11) whether this public health emergency declaration will again be extended. This has big implications for health insurance, health care delivery, and employers. Here are some of the major implications for employers.
a) Medicaid:
States have not been allowed (or required) to reestablish Medicaid eligibility during the pandemic. This means that some people who were eligible in 2019, for instance, would still be on Medicaid even if they lost eligibility due to having a higher income. About 25% more people are in Medicaid now than in early 2020. When the pandemic ends, states will again be allowed (and to some extent required) to do eligibility checks. Some estimate that as many as 15 million Medicaid beneficiaries (out of 80 million) will be disenrolled. The most likely to be disenrolled are working adults.
Here are links to more information on this from KFF (Kaiser Family Foundation) and the Commonwealth Fund.
Implications for Employers:
● Some employees who have waived insurance because they have remained on Medicaid will likely now want to utilize employer sponsored insurance
● Some employees will likely seek family plans after leaving their dependents on Medicaid through the pandemic
b) Telemedicine rules:
During the pandemic, Medicare has paid for telemedicine, and every state (and the District of Columbia) waived at least some telemedicine licensure rules. The federal government has also been lenient in sanctioning providers for HIPAA privacy violations (as long as their actions were in good faith). Some states have returned to pre-pandemic regulations and more will remove these changes when the pandemic emergency is over. At this point telemedicine makes up a majority of mental health visits in many plans. Proposals in Congress to extend these pandemic-era telemedicine rules face an uncertain future.
Implications for employers:
○ I expect that the national telemedicine vendors and virtual and digital care companies will be well-situated to continue to provide these services nationally.
○ Some providers are likely to cut back on their virtual care offerings, especially for out-of-state patients.
○ Telemedicine gained payment parity in many plans during the pandemic. However, many health plans are decreasing reimbursement rates since virtual visits have lower resource cost. This could further decrease access to virtual care.
c) Employee notice rules:
ERISA plans were instructed to ignore the pandemic time period (and 60 days after the pandemic ends) in calculation of certain COBRA and claims filing limits. The earlier COVID relief bill included COBRA subsidies which have since expired. Here is information about this issue from KFF (Kaiser Family Foundation). Look for the section on “other private insurance coverage flexibilities.”
Implications for employers:
● Employers should check with their compliance specialists to determine any changes needed in their policies and procedures when the pandemic emergency ends.
d) Federal payment for viral countermeasures:
The federal government is running out of pandemic funds to pay for vaccinations and antivirals. This is separate from the end of the declaration of the pandemic emergency. Congress could pass ongoing funding after the election, although it’s entirely possible that they will not, regardless of the results of the election. The Administration is talking about this as “commercializing” the vaccine and antiviral purchase. This will lead to a transfer of cost and risk to employers, and an increase in total costs.
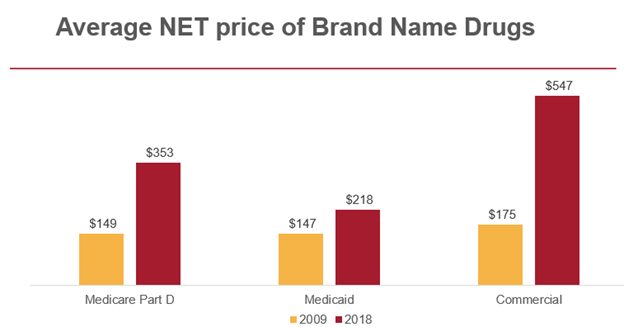
Here’s why. The feds are a “monopsony” purchaser (like a monopoly but on the purchasing side), and can therefore attain very advantageous prices. Pfizer has already announced that it expects COVID-19 boosters to sell for $110-130 per dose after “commercialization.” The federal government is now paying about $30 a dose. The federal government is paying about $530 per treatment course for Paxlovid – and the price is likely to increase when employers are purchasing this through Pharmacy Benefit Managers. Below is data published earlier this year by the Congressional Budget Office that shows prices in general are much higher for employer sponsored plans than for the government even after considering rebates.
Source: Congressional Budget Office, January, 2022 LINK The CBO has accounted for rebates in these prices.
Implications for employers:
- Expect higher prices for COVID vaccines and therapeutics in 2023! To give you a sense of this, if half of covered members get a $120 vaccine once a year, this is a cost of $60 per member per year, or $5 per member per month.
2. Paxlovid use associated with decreased risk of Long COVID-19
Researchers have extracted data from Veterans Administration electronic records, and shown that the risk of Long COVID was 26% lower among those who were diagnosed with COVID-19 and given Paxlovid compared to those who were not treated. The initial infections were from January to March, 2022, during the initial Omicron wave. Those who died within 30 days of diagnosis were excluded. Paxlovid was also associated with lower risk of hospitalization and death after the 30 day period, although these improvements did not reach statistical significance. The study included over 5600 veterans; about one in six were treated with Paxlovid. Average age was 65, and 86% of subjects were male.
Source: Xie, et al November 5, 2022 LINK
This is not a perfect study. The VA population is older and much more likely to be male than the overall population. Those in this research who got Paxlovid were less likely to come from a lower income zip code, and wealth is often associated with better outcomes. Interestingly, those treated with Paxlovid had higher rates of chronic heart and lung disease, and chronic disease has been associated with worse outcomes in other studies.
Implications for employers:
● Be cautious about initiating restrictions or prior authorization requirements for Paxlovid use once this drug is “commercialized” and the responsibility of employer-sponsored health insurance, especially since the drug must be started soon after the first symptoms to be effective.
3. Two new studies show the value of sick leave
The US is one of the few developed countries that has no requirement for employers to provide sick leave, although sick leave availability increased during the pandemic. Two new studies in this month's issue of the journal Health Affairs demonstrate the value of sick leave.
The first study shows that cities with sick leave mandates during 2021 achieved higher rates of COVID-19 vaccination among adults under 65, although there was no significant difference among adults over 65 (many of whom are no longer in the workforce). The impact was greatest in communities with a higher social vulnerability index, likely because higher paid workers were likely to have sick leave available even without a city mandate. The researchers adjusted for income and political leaning.
The second study, a longitudinal survey of over 60,000 shift workers for national chains, showed that women in geographies without a sick leave mandate were 11% less likely to report access to sick leave than men (43% vs. 54%). The researchers said that this gap remained even after adjusting for educational attainment and job tenure, and the gap was 8% when adjusted for part time employment status, and 5% when adjusted for industry sector. States and cities with sick leave mandates saw just about no gender gap in access to sick leave.
Implications for employers:
- Sick leave helps encourage workers not to come to the workplace when they are sick, and helps parents take care of sick children who are out of school.
- Sick leave can also be a component of inclusive employer policies to increase equity in the workplace.
Hope all have a great weekend.
Jeff