When hospitals affiliate with or purchase PCPs, costs and utilization rise
September 12, 2023
(Note: I will post COVID-19 update note tomorrow, since we’ll get news later today about CDC recommendations for who should get the new COVID-19 injection that should be available later this week)
Sinaiko, et al JAMA Health Forum September 1, 2023 LINK
Health care provider consolidation clearly increases provider leverage, and multiple studies have demonstrated that this consolidation raises medical costs. The increase in medical costs is most pronounced for private health plans; providers cannot use extra leverage to increase Medicare reimbursement since this is set by the Centers for Medicare and Medicaid Services.
Researchers at the Harvard School of Public Health analyzed medical claims of over 4 million members of private health plans in Massachusetts from 2013 to 2017 and compared the medical claims of primary care physicians that joined hospital systems in 2015 or 2017 to those which were never or always in hospital networks. During the study period, 4% of patients had a PCP who moved into vertical integration either by selling the practice or affiliating with a hospital for contracting purposes. Thirty four percent of patients had PCPs who were already vertically integrated in 2013, and 62% of patients were associated with PCPs who were not vertically integrated in 2017.
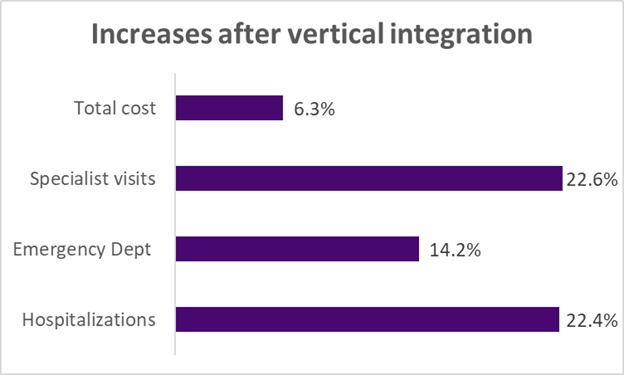
Those patients whose PCP became affiliated with a hospital system had more specialist visits, more emergency department visits, and higher annual costs compared to patients whose PCP did not affiliate during this time period. Patients whose PCP became affiliated with a hospital system during this study also were more likely to be hospitalized at a high-cost hospital, although this difference did not reach statistical significance. We do not know the “right” number of visits, so it’s possible that previously-independent PCPs offered too few visits before they became vertically integrated. There was no decrease in hospital readmissions, which the researchers suggested as a proxy for better coordination of care.
Implications for employers:
- Evidence continues to mount that consolidation in the provider community leads to increased costs.
- Antitrust enforcement can help, although the degree of consolidation in most markets is already quite high.
Employers can work with carriers on value-based design benefits that can help to steer patients to high-quality, lower cost health systems.
Tomorrow: Update on COVID-19
Thanks for reading. You can find previous posts in the Employer Coverage archive
Please “like” and suggest this newsletter to friends and colleagues. Thanks!

I agree - primary care physicians are relatively underpaid compared to other physicians - which is making it harder and harder to recruit new physicians into PCP training programs. There are some other reasons, too. The capital costs of running a "modern" practice are high- for instance it can cost $50K or more per physician to acquire and install electronic health records. Most med school graduates have enormous student debt, and therefore need to find a salaried job, as opposed to going into "private" independent practices. When older physicians who are the owners of independent practices want to retire - they are most likely to sell out to either hospitals or private equity because no one else will pay them as much for their practices, and the junior partners cannot afford to buy them out.
There's not a straightforward solution, but better antitrust enforcement could help, and many commentators feel that at the top end we need some sort of price caps so that hospital delivery systems cannot use their leverage to increase total reimbursement to unreasonable levels.
The excess cost of proceduralists being acquired by hospitals or by private equity companies is substantially higher than the cost of PCPs being acquired.
Thanks for the comment!
Maybe we should look at why this is occurring. If PCPs were reimbursed for the services they provide including caring for their patients maybe they would not feel the economic need to sell out to a system. We have a serious reimbursement disconnect for providers that needs to be fixed or we will continue to have irrational behaviors