Drug shortages continue to hamper care for cancer and ADHD
June 16, 2023 Updates on preventive care and COVID-19 vaccines, too
1. Drug shortages continue to hamper care for cancer and ADHD
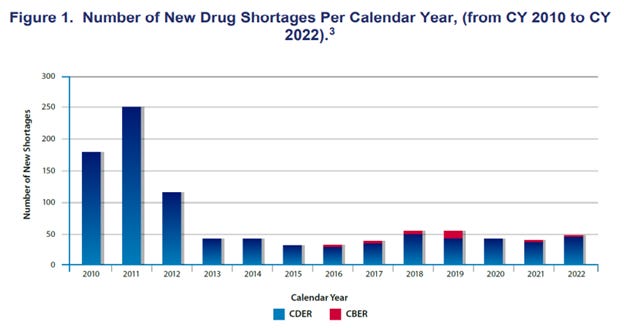
Source: Food and Drug Administration (FDA) June 7, 2023: Drug Shortages CY 22 LINK CBER is biologic drugs, and CDER is all other medications. Eighty non biologics and 6 biologics are in “ongoing” shortage according to the FDA.
We go from emergency to emergency in drug shortages. Last fall, we were short of antibiotics used frequently for upper respiratory tract infections, as well as over the counter acetaminophen (Tylenol) for children. This spring, we are plagued with shortages of cisplatin and carboplatin, key ingredients in potent chemotherapy cocktails. Without these drugs, patients with cancer face higher mortality. Those with Attention Deficit Disorder and Hyperactivity have been hard-pressed to find the medications that help them modulate their attention and behavior. Penicillin G, used for treatment of syphilis, is also in short supply.
There are many causes of drug shortages. Most drugs which are in short supply are generic medications that are quite low cost. Ongoing competition to lower costs has led to most generics being manufactured overseas where overhead costs are lower than in the US. The payment for these medications is low enough that new companies will not enter the market to manufacture them, leaving just a few sources. Existing manufacturers will often shut down production if they have to make new capital investments in their plants. In some instances, shortages have begun when the FDA has banned imports from plants which have failed safety inspections.
I usually write about excessively high prices, but this is an instance where exceptionally low costs are leading to supply challenges. A reliable supply of reasonably priced generic medications would lead to better outcomes and less disruption of medical care than a fragile supply of drugs at rock-bottom prices. For instance, the FDA frequently discovers poor quality controls at manufacturing plants in India, but there are few alternative manufacturers. Efforts to produce high quality generics in the US will only succeed if manufacturers are paid sustainable prices and the generics are widely used.
Implications for employers:
- Employers can instruct their pharmacy benefit managers to be flexible about formulary lists, out of pocket costs, and prior authorization in instances where a preferred drug is unavailable and delay in care could lead to adverse health outcomes.
- We should expect higher prices for some generics to be sure that there is margin for multiple competing manufacturers; the alternative is that all but one or two manufacturers will leave the market, and we could face both shortages and excessive inflation.
Two Brief Updates:
Preventive care mandate will remain in place for now
The Biden Administration and the plaintiffs who sued to invalidate the Affordable Care Act mandate to offer preventive care without cost sharing reached a tentative agreement this week (after being instructed to do so by the federal appeals court hearing the case). This agreement will keep the preventive mandate in place pending the Circuit Court of Appeals ruling, which is expected to come after open enrollment season for most employers this fall. This case is also likely to be appealed to the Supreme Court, so the mandate is likely to remain in place for quite a while. In exchange for keeping the mandate in place, the Administration has agreed not to prosecute the plaintiffs for not covering preventive care recommended by the US Preventive Services Task Force after March, 2020.
For more details see this post from April.
Implication for employers:
· The preventive care mandate remains in effect for all but a handful of employers who brought this case to court.
The FDA’s Advisory Committee unanimously endorsed a revised COVID-19 vaccine for the fall
The new vaccine will be targeted to an Omicron strain that is now dominant, and will no longer include the original strain from 2020, which is no longer in circulation. This unanimous recommendation is still to be reviewed by the FDA and the Centers for Disease Control and Prevention, and we don’t yet know who will be recommended for vaccination. This will be the first COVID-19 vaccine that must be privately purchased by employer sponsored health plans, as the government no longer has funding for COVID-19 vaccines.
Implication for employers
· Stay tuned for details, and it is possible that there will be COVID-19 vaccines to include in fall influenza vaccine clinics.
· It’s previously been reported that COVID-19 vaccines will likely cost about $120 per dose when purchased privately.
Monday’s post will be about research on the LGBTQ+ health insurance gap