Employers seeking cost saving programs, mental health care can lower medical spending, maternity care post-Dobbs, and current COVID-19 status.
January 6, 2023
Happy New Year, and Happy Friday!
Today, I’ll review various approaches to lowering employer medical costs, discuss a study associating prompt behavioral health care with lower medical claims costs and maternity care resource issues after the Dobbs decision. I’ll also share some thoughts on current COVID-19 and influenza status as the new variant XBB.1.5 continues to grow.
1. How employers can lower medical costs
Medical cost inflation is the highest it’s been in over a decade, due to a combination of overall inflation, provider consolidation, and medical progress. We expect costs to increase further over the next two years, as many health plan multiyear contracts are renegotiated. This represents a challenge to employers offering health insurance, who are already buffeted by other rising costs and the threat of an economic downturn.
Source: WTW Best Practices Survey, 2022 LINK
There are three basic ways employers can lower health care costs.
(1) Have fewer covered members, either by decreasing headcount or shifting employees or dependents to other plans or the individual marketplace if they are eligible for federal subsidies.
(2) Decrease company-provided subsidization, shifting more premium or out-of-pocket costs to employees. This could adversely impact recruitment and retention given the current labor shortage, and many employees already face high total medical costs even if they have employer-sponsored health insurance.
(3) Increase health care efficiency, by having healthier employees, using higher value providers, having better contracts or having better medical management programs. It’s not always easy or quick to increase health care efficiency, but efforts here can pay large dividends. Health care costs in the US are higher than elsewhere mostly due to high prices rather than overutilization. Therefore, employers should have some focus on unit prices.
Employer characteristics determine which employers can benefit from which programs or initiatives. For instance, smaller employers face high costs of contracting for programs separately with multiple vendors and are more likely to benefit from programs offered through their health plan carrier or pharmacy benefit manager. Demographics of a population matter, too! An employer with a large portion of younger employees might benefit more from a program to improve fertility and maternity care, and an employer with a high average age might give more consideration to a program for congestive heart failure or chronic obstructive pulmonary disease. Employees with high rates of diabetes or kidney disease could benefit most from programs to address members with these conditions.
There is a huge difference in provider unit price, and this is usually unrelated to quality or outcomes. Therefore, centers of excellence (COE) or high-performance network programs which direct members to the highest value providers can provide large cost savings. Some COEs also offer bundled prices. These programs are most effective with substantial financial incentives, but which should be carefully developed to balance member and company cost impacts. Site of care matters, too. Programs to steer patients to ambulatory care centers for infusions and surgery can also decrease costs compared to care at hospitals.
Costs for newly approved brand name pharmaceutical products continue to increase rapidly, even as costs for generic drugs continue to decline. Utilization management programs to be sure these drugs are being used prudently can lower costs. Programs to use manufacturer coupons to lower employer costs have been controversial, although can lead to large short-term cost savings. There will be new biosimilars for some expensive biologic brand name anti-inflammatory drugs in 2023 and beyond, which should lead to cost savings. Savings for biosimilars will not be as large as discounts for generic “small molecule” drugs, since the cost of production for biologics is substantially higher.
Many look to preventive care to lower total health care costs, but only childhood vaccinations and birth control save very substantial medical claims costs; most other preventive care provides longer or better quality life at a reasonable cost (but no net cost savings). Tobacco cessation programs can decrease costs modestly, and encouraging lower cost colorectal cancer screening (FIT tests rather than colonoscopy) could lower costs and increase the acceptability of screening.
Most medical costs are incurred by a small number of plan members; 1% of the population is responsible for over 20% of costs, and 5% of the population represents 50% of total costs. Diligent nurse care management of this group can decrease complications and lower health care costs.
For some employers, review and reprocurement of health plan or pharmacy benefit manager can be a source of savings, although this is a process that usually takes over a year.
Implications for employers:
- The next few years will likely be difficult in terms of total health care costs, but targeted efforts can help control the rate of increase in employer costs while maintaining health care affordability for employees and their families.
- Employers should focus their efforts based on the demographics and claims experience of their covered population.
2. Prompt behavioral health care associated with lower medical costs
Individuals with a chronic mental health condition have, on average, higher total medical expenses. Now a new study suggests that early treatment of mental health conditions can effectively lower costs.
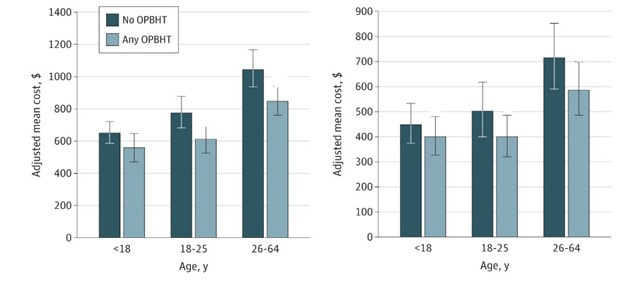
Researchers from Evernorth, a division of CIGNA, reviewed medical claims of over 200,000 patients who had a new medical claims mental health diagnosis (not seen in the previous 12 months). They found that those who saw a behavioral health clinician at least once within thirty days of this diagnosis had lower medical costs than those who never saw a behavioral health clinician. Their research was published last month in JAMA Network Open.
The researchers followed almost 75,000 of those patients for 27 months; again those with at least a single behavioral health clinician visit had lower costs than those who had no such visit. The researchers adjusted for previous illness, demographics, and a host of other factors, and those with behavioral health visits continued to have lower expenses. As with all studies of medical claims, coding is likely inaccurate in some instances, and those with a mental health issue who got no medical care would not be included. The researchers also excluded members who did not have continuous medical and pharmacy coverage beginning 12 months prior to the study period.
In this study, only 44% of plan members had an outpatient behavioral health visit within 30 days of diagnosis.
Medical claims costs at 15 months Medical claims costs at 27 months
Source: Bellon, et al JAMA Network Open, 12/6/22 LINK
Implications for employers:
- Access to mental health services is important for clinical reasons. Those with depression, anxiety, or substance use disorder do better when they are treated by mental health specialists.
- This study suggests that we might see some claims cost reductions from prompt treatment of mental illness, too.
- We hope that increased mental health access through virtual visits will help more people get prompt care. This study time period was pre-pandemic, when virtual care in mental health was rare.
3. Maternity care resources lower in states that are now restricting abortion
The Commonwealth Fund published data last month that showed that there are about a quarter fewer obstetricians andmidwives in the 26 states that have banned or restricted abortions compared to states without such restrictions. The report also shows that these states on average had poorer maternity outcomes than states which have not restricted abortion prior to the Dobbs decision.
Source:DeClercq, et al Commonwealth Fund, 12/22 LINK
Implications for employers:
- Many employers have sought approaches to maintain member access to abortion services immediately after the Dobbs decision allowed states to ban or severely restrict abortion access.
- Employers and health plans should monitor access to maternity care. If many who would have otherwise had abortions carry their pregnancies to term, many states might see a shortage in maternity capacity.
- DEI strategies should take into account the increasingly disparate reproductive services available to women.
4. COVID-19 cases expected to continue to climb
Many of us enjoyed recreational travel over the holidays. Restaurants, movies, and live shows are back. But the news reminds us that the immune-evasive Omicron variant XBB is rapidly becoming dominant, and the number of cases, hospitalizations, and deaths from COVID-19 is on the rise. The end of the “Zero COVID” policy in China has led to a large outbreak, and some believe this will lead to even more variants and could have an impact on global supply chains.
This fall we’ve had exceptionally high levels of RSV (respiratory syncytial virus) and flu (influenza), and the rate of COVID-19 infections has not declined. That’s why it’s hard to find children’s acetaminophen or adult multi-cold medicine on the shelves, and why rates of workplace absence have spiked. The RSV spike has subsided; influenza rates remain higher than in previous years, but are decreasing; COVID-19 test positivity, hospitalization and death rates are increasing. Wastewater monitoring shows an increase in coronavirus across the country and appears worst in the northeast.
The new XBB variant and its XBB.1.5 subvariant now represent about half of the cases of COVID-19 in the US. These seem better able to evade immunity from past vaccination or infection, although do not seem to cause more severe disease. It will be months before we know the impact of this new variant on Long COVID.
Implications for employers:
- We continue to have tools to address this threat! The bivalent booster has been shown to decrease risk of hospitalizations, and Paxlovid treatment has been shown to reduce risk of hospitalization, death, and Long COVID.
- High quality mask use and better indoor air quality reduces risk of transmission of all respiratory viruses. Handwashing reduces risk of RSV and flu.
- Actions employers can take include
- Continue to strongly recommend influenza and COVID-19 vaccination.
- Offer paid time off to encourage workers with respiratory illness to stay home
- Improve indoor air quality - which protects against all respiratory viruses and also can increase productivity and wellbeing. This can include increased ventilation or filtration, and often does not require large capital investments.
- Make the workplace mask friendly. Few employers outside of health care will mandate mask use, but employees should feel comfortable wearing masks for any reason. Many are likely to want to wear masks indoors, including those who are or live with others who are older or immunocompromised.
- Offer virtual or remote options, especially while rates of respiratory infections are high.
- Encourage home testing for those who have been exposed, and for those who are about to travel, or have just returned from traveling. Employees can still get 8 home COVID-19 tests per beneficiary monthly through their employer-sponsored health insurance plan.
Hope that all had a wonderful holiday season, and best wishes for a joyous, fulfilling and healthy new year!