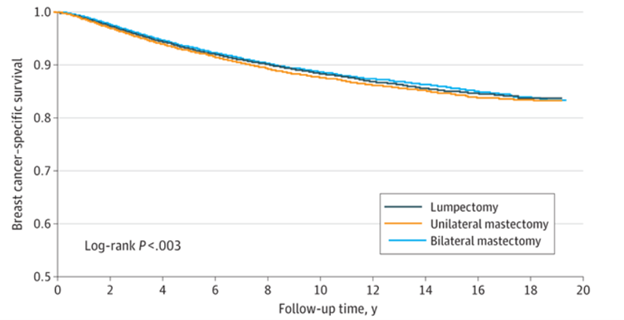
A) Bilateral mastectomy decreases cancer recurrence, but not death from metastatic breast cancer
20-year breast cancer survival
Source: Giannakeas, et al JAMA Oncology July 25, 2024 LINK This shows that 20 years after breast cancer diagnosis over 80% (0.8 on “y” axis) of patients were still alive.
Women with newly diagnosed breast cancer in one breast often ask their doctors if they should have both of their breasts removed to lower their chances of recurrent cancer. Last week, JAMA Oncology gave an answer – at 20 years post-treatment, there was no survival difference between a lumpectomy, single mastectomy, or double mastectomy for women with breast cancer which has not spread. This was a large observational study, with over 100,000 women followed for two decades.
Some women with newly diagnosed breast cancer will continue to choose double mastectomies. While double mastectomy does not improve survival it lowers the chances of breast cancer in the opposite breast. However, many women will also choose single mastectomies or lumpectomies and this research provides them with reassurance. The decision on best therapy should be made by the patient in consultation with a treating oncologist, and genetic characteristics of the cancer play a large role in treatment recommendations. We need further research on this topic, and employers should cover genetic testing for people with breast cancer, and should not make any changes in their benefit design based on this study.
B) Twice-yearly PrEP therapy is highly effective
The New England Journal published research last week that demonstrated that lenacapaviras pre-exposure prophylaxis (PrEP), is very effective in preventing HIV infections. Lenacapavir (Sunlenca) is currently used for treatment of resistant HIV, and its list price is $39,000 a year. The study participants were young cis-women in Uganda and South Africa where background rate of HIV infection among women is high. The drug was tested in a randomized double blind trial against emtricitabine–tenofovir alafenamide (Truvada), and daily oral emtricitabine–tenofovir disoproxil fumarate (Descovy).
Drugs that are injected twice a year are likely to have higher adherence rates, and it’s heartening that not a single person in the lenacapavir group (1939 patient-years) was infected. On the other hand, this drug is very expensive, and some clinicians are now prescribing “on demand” pre-exposure prophylaxis that might be appropriate for those who have high-risk sexual encounters less frequently. We need more agents with different characteristics to make HIV a rare disease over the coming years, so this is good news.
Here are links to past posts on PrEP.
C) Interest high in compounded GLP-1 medication
Interest continues to grow in compounded GLP-1 anti-obesity medications. Most are being sold directly to consumers, and compounded medications are only allowed by the FDA because the branded medications are currently in short supply. Here’s a link to a KFF article on this, and an FDA alert. Compounded GLP-1 medications generally come in multi-dose vials and are injected by a syringe, so there is more opportunity for patient error in dosing or administration than with brand name GLP-1 pens.
D) PBM reports low levels of persistence with GLP-1 medications
Prime Therapeutics released research from its pharmacy claims which showed that 85% of continually enrolled plan members who started on a GLP-1 medication were not on that medication two years later. About a quarter of those (26%) who started one GLP-1 medication switched to a different GLP-1 medication. When people stop GLP-1 medications they generally regain a substantial portion of lost weight.
It’s not clear from this report whether those who stopped the medication had reached their goal, were troubled by side effects, or had affordability or insurance barriers to continued therapy. Some who discontinued the medication might have appeared to stop because they decreased frequency of injection, or they might have obtained medication from a compounding pharmacy or from abroad.