USPSTF gives “A” rating to drugs to prevent spread of HIV
September 7, 2023
The US Preventive Services Task Force (USPSTF) has reaffirmed its “A” rating for PrEP, pre-exposure prophylaxis, to prevent HIV infection in those at high risk. This requires employer sponsored health plans to cover PrEP and associated office visits and laboratory tests, although there is litigation which could eliminate this requirement. When the USPSTF first addressed this issue in 2019, there was only a single medication, Truvada (emtricitabine-tenofovir), approved for preexposure prophylaxis. Now, there are three medications approved. Truvada (a generic version is now available), Descovy (also emtricitabine with a different variety of tenofovir), and Apretude (cabotegravir), a drug which is administered every other month by an injection at a provider’s office.
PrEP is an important component of the national plan to sharply reduce or eliminate HIV transmission, which could make HIV/AIDS a rare disease in another generation. PrEP is 99% effective at preventing sexually transmitted HIV, and 74% effective at preventing HIV transmission from intravenous drug use. However, there are huge disparities in the use of PrEP. Black people and Hispanic people represent a majority of those newly diagnosed with HIV, but only a minority (9% and 18% respectively) of those are on PrEP.
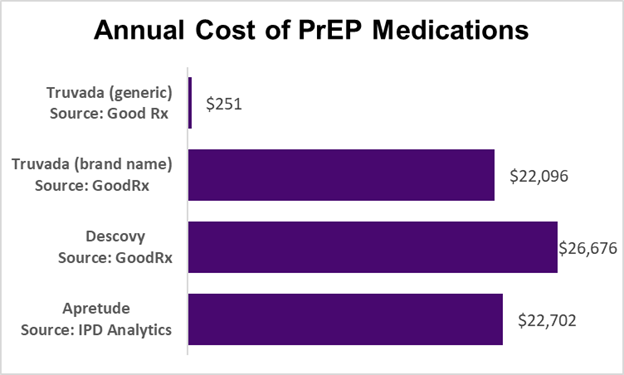
Many advocates are calling on the government to mandate coverage of all types of PrEP therapy, noting that for some people at risk, an injection six times a year might lead to higher adherence than a daily pill, and the generic medication is not indicated for those with kidney dysfunction or osteoporosis. A challenge is prices for these medications.
Apretude is administered as an intramuscular injection at a provider office. This is drug cost only.
At this point, generic emtricitabine-tenofovir (Truvada) is covered with no cost sharing by most employer plans, although Descovy might be approved for $0 copay with documentation of poor kidney function or osteoporosis. Brand name PrEP medications are generally covered but at Tier 3 cost sharing and some formularies might not offer coverage at all. Drugs that are effective for PrEP are also often used for treatment of HIV infection, in which case there is member cost sharing.
Implications for Employers:
- Emtricitabine-tenofovir is widely available as a low-cost generic. This drug and associated laboratory tests and office visits should be covered without cost sharing as preventive services
- Other PrEP medications are available only as brand names and are very expensive. Although they might be preferred for a small portion of members at high risk of HIV, most employers will choose to only cover these expensive brand name medications with cost sharing or with documentation of specific medical conditions where the generic drug is not appropriate.
Thanks for reading. You can find previous posts in the Employer Coverage archive
Please “like” and suggest this newsletter to friends and colleagues. Thanks!