Summary: Cervical cancer incidence and mortality is declining due to HPV vaccines and screening, but rural and Black women have higher rates of cervical cancer
Source: Amboree, et al JAMA Network Open March 3, 2025
Most cases of cervical cancer are preventable by vaccination against Human Papillomavirus (HPV) or can be found and treated early before they are invasive through screening with pap smears and HPV testing. Indeed, the overall incidence and mortality of cervical cancer is decreasing.
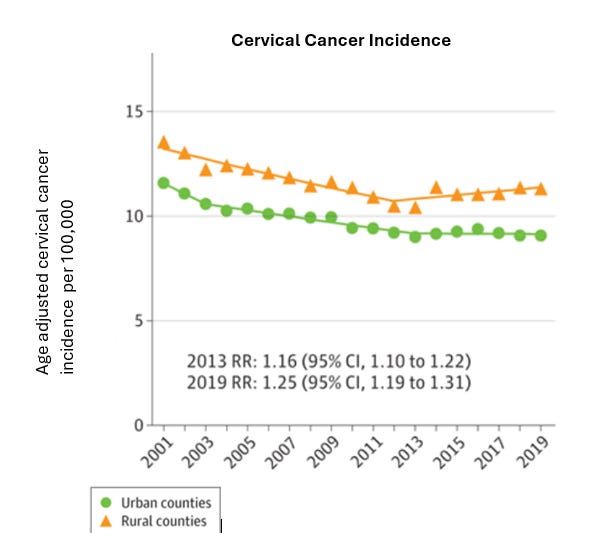
However, research published this month in JAMA Network Open demonstrates that rural and minoritized populations continue to suffer disproportionately from invasive cervical cancer. Women in rural counties had a 25% higher incidence of cervical cancer and a 42% higher risk of mortality. In fact, rates of cervical cancer incidence increased in rural counties from 2012-2019, and Black women have mortality rates significantly higher than White women.
Source: Amboree, et al JAMA Network Open March 3, 2025
(Numbers calculated from published graphic using plotdigitizer.com)
Rural counties have increasingly become “maternity deserts” where there are no obstetrical services available, and screening for cervical cancer is likely to become more difficult to obtain in these counties. Further, rural areas in states which have restricted abortion might have fewer women’s health clinics, which are a major provider of cervical cancer screening. Approval of the at-home test for cervical HPV infection could help maintain screening rates in areas with less access to gynecologic care.
Here's a link to a previous post on the excellent effectiveness of HPV vaccine in preventing invasive cervical cancer.
Implications for employers:
● Employers can ask their carriers for reporting on the rate of HPV vaccination among teenage boys and girls as well as rates of cervical cancer screening.
● Employers can communicate with their members that HPV vaccination is covered with no cost sharing.
● Employers can ask their carriers to provide reimbursement for self-testing for cervical cancer when this is approved by the FDA.
● Identifying groups at highest risk for various bad health outcomes helps companies design more effective programs to improve population health.
Thanks for reading. You can find previous posts in the Employer Coverage archive
Please subscribe, “like” share this newsletter with friends and colleagues. Thanks!
Tomorrow: Workers express both fear and excitement about AI